WikiJournal of Medicine/Reference ranges for estradiol, progesterone, luteinizing hormone and follicle-stimulating hormone during the menstrual cycle
WikiJournal of Medicine
Open access • Publication charge free • Public peer review • Wikipedia-integrated
This article has been through public peer review.
Post-publication review comments or direct edits can be left at the version as it appears on Wikipedia.First submitted:
Accepted:
Reviewer comments
PDF: Download
DOI: 10.15347/wjm/2014.001
QID: Q44275619
XML: Download
Share article
![]() Email
|
Email
| ![]() Facebook
|
Facebook
| ![]() Twitter
|
Twitter
| ![]() LinkedIn
|
LinkedIn
| ![]() Mendeley
|
Mendeley
| ![]() ResearchGate
ResearchGate
Suggested citation format:
Mikael Häggström (2014). "Reference ranges for estradiol, progesterone, luteinizing hormone and follicle-stimulating hormone during the menstrual cycle". WikiJournal of Medicine 1 (1). doi:10.15347/WJM/2014.001. Wikidata Q44275619. ISSN 2002-4436. https://upload.wikimedia.org/wikiversity/en/0/05/Reference_ranges_for_estradiol%2C_progesterone%2C_luteinizing_hormone_and_follicle-stimulating_hormone_during_the_menstrual_cycle.pdf.
Citation metrics
AltMetrics
Page views on Wikipedia
Wikipedia: Content from this work is used in the following Wikipedia article: Estrogen, Estradiol, Menstrual cycle, Ovulation, Reference ranges for blood tests, Progesterone, Follicle-stimulating hormone, Luteinizing hormone.
License: ![]() This work is released into the public domain by the copyright holder (under a CC0 license). This applies worldwide. Any person may use this work for any purpose, without any conditions, unless such conditions are required by law.
This work is released into the public domain by the copyright holder (under a CC0 license). This applies worldwide. Any person may use this work for any purpose, without any conditions, unless such conditions are required by law.
Mikael Häggström ![]() (handling editor) contact
(handling editor) contact
Article information
Abstract
Figures
Interpretation
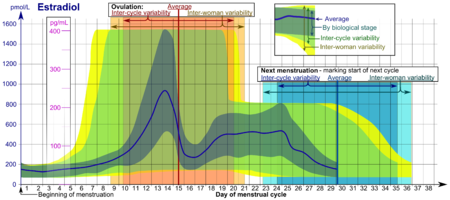
The time scale starts with the beginning (or "onset") of (last) menstrual period (LMP), given as day number. Day number 1 corresponds to 0 to 0.99 days from the beginning of the LMP, and Day number 2 corresponds to 1.00 to 1.99 days from the beginning of the LMP and so forth. The time scale ends at whatever is the actual next menstruation, which marks the beginning of the next cycle, which is equivalent to starting all over again from the beginning of the time scale.
- Inter-cycle (also called within-woman or intrawoman) variability for ovulation and next menstruation are the 95% prediction intervals for the timing of these events in any single woman, assuming an inter-cycle average duration that is equal to population average.
- Inter-woman variability for ovulation and next menstruation are the 95% prediction intervals for the timing of these events in the overall population.
Hormone levels represent usual ones, not necessarily related to what is healthy. Hormone ranges vary between cases at the same biological stage of the menstrual cycle. Furthermore, the actual timing (usually given in day numbers from mentruation) of that biological stage varies, both between cycles of any single woman (inter-cycle) and between somen (inter-woman). Therefore, the appropriate ranges to use depend on how certain the actual biological stage can be estimated at any time.
- The levels denoted Average refer to the (arithmetic) means for hormone levels.
- The ranges denoted By biological stage are the 90% prediction intervals for hormone levels for women at the same biological stage. These reference ranges may be used in closely monitored menstrual cycles in regard to other markers of its biological progression, with the time scale being compressed or stretched to how much faster or slower, respectively, the cycle progresses compared to an average cycle. In the luteal phase, a known time of ovulation is sufficient to use these ranges.
- The ranges denoted Inter-cycle variability (also called within-woman or intrawoman variability) are the up to 95% prediction intervals for any single woman, assuming an inter-cycle average duration that is equal to population average. These ranges are more appropriate to use in non-monitored cycles with only the beginning of menstruation known, but where the woman accurately knowing her average cycle lengths and time of ovulation, and that they are somewhat averagely regular, with the time scale being compressed or stretched to how much a woman's average cycle length is shorter or longer, respectively, than the average of the population.
- The ranges denoted Inter-woman variability are the up to 95% prediction intervals for hormone levels in the overall population. These ranges are more appropriate in non-monitored cycles, where the average cycle lengths and time of ovulation are unknown, but only the beginning of menstruation is given.
Derivation
Average hormone values
The average hormone levels are taken from Stricker 2006,[1] with some regression to a smoother curve between values of a rather zigzag pattern. The confidence intervals for the average values are not given in this study, however. The data from Stricker 2006 uses the LH peak as the reference point, which in the following sections will be adjusted to the more commonly used reference point of the beginning (or "onset") of (last) menstrual period.
Average time of ovulation
The time of ovulation is an average between that expected from the LH peak and that expected from the estradiol peak, with intervals taken from Pauerstein 1978. "The mean interval from the estrogen peak to ovulation was 34 hours, the interval from the estrogen peak to the LH peak was 24 hours, and that from the LH peak to ovulation was 9 hours." [2] The estradiol peak, in turn, is estimated from computer-generated regression between the two average estradiol measurements of highest value. As a result, average time of ovulation is calculated to be almost exactly between 0 and 1 day from LH peak as given in Stricker 2006[1].
Beginning of menstrual cycle
The beginning of menstruation, which is taken as the limit between one cycle and the next, is subsequently taken as 14.6 days prior to average time of ovulation, according to Geirsson 1991.[3] Resultantly, the beginning of menstruation occurs almost exactly at the point minus 14 days from LH peak in Stricker 2006.
Ovulation variability
The 95% inter-cycle prediction interval of the ovulation of 9.4 to 19.6 days after menstruation is derived from a standard deviation in this interval of 2.6, as given in Fehring 2006[4] (using the term "intrawoman") for the follicular phase, which in this study marks the interval between menstruation and ovulation. It cites: "the mean intracycle length difference of the follicular phase (5.8 days, SD = 2.6)".
The 95% inter-woman variability is provided by Geirsson 1991,[3] giving 8.2 to 20.5 days after beginning of menstruation.
The confidence intervals for the time of ovulation are not given.
Cycle length
The average duration of a menstrual cycle is measured to be 29.1 days[5] (not 28 as commonly given). The same study that gives the average of 29.1 also states that the value could intentionally be decreased to appear to be around 28 by excluding individuals above or below certain cycle lengths, but as such exclusion limits are largely arbitrary, this diagram uses the value of the entire study population.
Average hormone levels at extremities
In Stricker 2006,[1] readings are only up to 28.0 days after LMP. However, the value of 0 days after LMP can be regarded as equivalent to the value 29.1 days after LMP, assuming that a menstrual cycle begins as it ends. Furthermore, its first reading (- 15 days from LH peak), is actually - 1 day from the standard start of the menstrual cycle (LMP), and is therefore moved to the other side of the diagram, that is, to 28.1 days after LMP. In between, lines are adjusted to an approximate average of that expected from the ones coming from the upper and lower extreme, with additional change in curve angles as far back as 26.0 days after LMP and forward as far as 1.0 days after LMP.
Cycle length variability
The 95% inter-cycle prediction interval for the subsequent ovulation of 23.6 to 34.6 days after last menstruation is derived from an equivalent standard deviation of 2.8, as given in Liu 2004[6] (using the term "within-woman"). The 95% inter-woman prediction interval of 22.3 to 35.9 days after last menstruation is derived from a standard deviation of 3.5, from the same study.[6] It cites: "the between-woman standard deviation was 3.45 days and the within-woman standard deviation was 2.84 days for mean cycle length, based on 943 cycles."
Hormone ranges by biological stage
Hormone ranges by biological stage are taken directly from data in Stricker 2006,[1] with adjustment at extremities as with average hormone levels.
The lower limit was given as the 5th percentile, and the upper as the 95th percentile, resulting in a 90% prediction interval.
The Stricker study synchronizes days with the LH peak, but this, in turn, is approximated to have reliably constant time intervals both to other hormone levels as well biologic processes around ovulation, so relation between biological stage and hormone levels is approximated to be reliably constant as well. As a consequence of this approximation, these ranges may be less accurate in representing levels at biological stage at the extremities, that is, far from the time of ovulation.
Besides from such uncertainty, the resultant ranges in the follicular phase correspond to the case of an exact prediction of the ovulation, as the follicular phase ranges are given in retrospect.
In the luteal phase (after ovulation, until beginning of next menstruation), the given ranges represent the case where only ovulation is known, as was essentially the case in the source study.[1] However, the difference from actual ranges by biological progression is relatively minor, since the inter-cycle and inter-woman variabilities are substantially smaller in the luteal phase than in the follicular phase:
- The inter-cycle variability in the luteal phase roughly corresponds to the difference of the total cycle inter-cycle variability (standard deviation 2.8, given by Liu 2004[6] and the follicular phase inter-cycle variability (standard deviation of 2.6, as given in Fehring 2006[4]) resulting in a standard deviation of 0.2 days.
- Similarly, the inter-woman variability in the luteal phase roughly corresponds to the total cycle inter-woman variability (standard deviation 3.5, given by Liu 2004[6] and the follicular phase inter-woman variability (standard deviation of 3.1, as estimated from a 95% prediction interval of 8.2 to 20.5 given in Geirsson 1991[3]) resulting in a standard deviation of 0.4 days.
Inter-cycle and inter-woman ranges
Inter-cycle and inter-woman ranges are approximated by horizontal widening of the ranges by biological stage with the inter-cycle and inter-woman variability in timing, respectively. These horizontal variabilities, in turn, are approximated to increase linearly from beginning of the cycle to ovulation, and again linearly from ovulation to the next menstruation. Subsequently, as the source studies did not directly measure the 95% prediction intervals of hormone values from the time of last menstruation, the approximation used for these diagrams expand beyond such a direct measurement. An extreme example of this a hormone value at the upper limit of the 95% prediction interval by biological stage, occurring at the earliest limit in the 95% prediction interval of time of ovulation, which when taking both variables together would occur on the 99.75% prediction interval, because surpassing that limit would require being at the extremes of both hormonal levels by the same biological stage and the timing of that stage. In fact, in locations where the prediction intervals by biological stage form clear peaks, the addition of equivalent variability in timing would likely yield a numerically lower maximal timing because of spread-out. A likely adverse effect of this would be a apparently narrower reference interval by biological stage for women who actually have very averagely timed cycles, an effect which favors actually rather having a wider prediction interval than 95% when adding variability in timing, such as is the case in this diagram.
This approximation also assumes that there is no correlation between cases of far-from-average levels in hormones at a specific biological stage and cases with far-from-average timing of that biological stage. Such a correlation would narrow down the inter-cycle and inter-woman ranges.
Reference list
- ↑ 1.0 1.1 1.2 1.3 1.4 Stricker, Reto; Eberhart, Raphael; Chevailler, Marie-Christine; Quinn, Frank A.; Bischof, Paul; Stricker, René (2006). "Establishment of detailed reference values for luteinizing hormone, follicle stimulating hormone, estradiol, and progesterone during different phases of the menstrual cycle on the Abbott ARCHITECT® analyzer". Clinical Chemical Laboratory Medicine 44 (7). doi:10.1515/CCLM.2006.160. ISSN 1434-6621..
- Excel file of data is available at: https://docs.google.com/open?id=0B8IdyPbSsy9rNlRfTU1USDhkUTA
- ↑ Pauerstein CJ, Eddy CA, Croxatto HD, Hess R, Siler-Khodr TM, Croxatto HB (April 1978). "Temporal relationships of estrogen, progesterone, and luteinizing hormone levels to ovulation in women and infrahuman primates". Am. J. Obstet. Gynecol. 130 (8): 876–86. doi:10.1016/0002-9378(78)90264-8. PMID 416719. http://www.ncbi.nlm.nih.gov/pubmed/416719.
- ↑ 3.0 3.1 3.2 Geirsson RT (May 1991). "Ultrasound instead of last menstrual period as the basis of gestational age assignment". Ultrasound Obstet Gynecol 1 (3): 212–9. doi:10.1046/j.1469-0705.1991.01030212.x. PMID 12797075. [2]
- ↑ 4.0 4.1 Fehring RJ, Schneider M, Raviele K (2006). "Variability in the phases of the menstrual cycle". J Obstet Gynecol Neonatal Nurs 35 (3): 376–84. doi:10.1111/j.1552-6909.2006.00051.x. PMID 16700687.
- ↑ Chiazze L, Brayer FT, Macisco JJ, Parker MP, Duffy BJ (February 1968). "The length and variability of the human menstrual cycle". JAMA 203 (6): 377–80. doi:10.1001/jama.1968.03140060001001. PMID 5694118. http://jama.ama-assn.org/content/203/6/377.abstract.
- ↑ 6.0 6.1 6.2 6.3 Liu Y, Gold EB, Lasley BL, Johnson WO (July 2004). "Factors affecting menstrual cycle characteristics". Am. J. Epidemiol. 160 (2): 131–40. doi:10.1093/aje/kwh188. PMID 15234934.