WikiJournal Preprints/Immune system
This article is an unpublished pre-print undergoing public peer review organised by the WikiJournal of Medicine.
It is adapted from the Wikipedia page Immune system. It contains some or all of that page's content licensed under a Creative Commons Attribution ShareAlike License and will also be used to update that article after peer review.You can follow its progress through the peer review process at this tracking page.First submitted:
Reviewer comments
QID: Q116734788
Suggested (provisional) preprint citation format:
Sarmoko; Muhammad Novrizal Abdi Sahid. "Immune system". WikiJournal Preprints. Wikidata Q116734788.
License: ![]()
![]() This is an open access article distributed under the Creative Commons Attribution ShareAlike License, which permits unrestricted use, distribution, and reproduction, provided the original author and source are credited.
This is an open access article distributed under the Creative Commons Attribution ShareAlike License, which permits unrestricted use, distribution, and reproduction, provided the original author and source are credited.
Roger Watson ![]() contact
contact
Article information
Abstract
Introduction
[edit | edit source]The immune system is a host defense system that includes many biological structures and processes within an organism that protects against disease. In many species, the immune system can be classified into subsystems, such as the innate immune system and the adaptive immune system. These processes include phagocytosis, complement system, and the synthesis of antimicrobial peptides. Human has much more complex defense mechanisms, including the ability to adapt to more accurately recognize pathogens.
The immune system employs a range of mechanisms to protect the host. Physical barriers serve as the first line defense, preventing pathogens from entering the body.[1] However, if pathogens manage to breach these barriers, they encounter the innate immune system, that can provide rapid responds to eliminate the pathogens. When pathogens effectively resist the innate response, the adaptive immune system is activated and tailored to address the specific threat.[2] This response involves the production of lymphocytes, which act as effector cells capable of destroying pathogens as well as generating antibodies. During an infection, the immune system adapts its response then maintained after the pathogen has been eliminated, including the formation of lymphocyte memory, which allows for a more rapid and potent reaction upon subsequent encounters with the same pathogen.[3][4]
Innate immune system
[edit | edit source]Microorganisms or toxins that successfully enter the body encounter the cells of the innate immune system. The innate response is typically activated when microbes are identified by receptors that recognize molecules that are conserved among broad groups of microorganisms,[5] or molecules that released from damaged cells.[6]
Surface barriers
[edit | edit source]The organisms cannot be completely sealed from their surroundings, thus the mechanisms act to protect the openings of the body, such as the lungs, intestines, and the genitourinary tract. Several barriers, including mechanical, chemical, and biological barriers, protect organism from infection. Surface barriers are part of mucosal immunity, which formed in the mucosal area by the mucosal ecosystem. The mucosal area covers a much larger body surface compared to the skin area. Each mucosal area is consists of slightly different immune components that affect their primary mechanism of response toward pathogen invasion.[7]
The mucosal immune system components are the physical barrier, humoral component, cellular component, and gut microbiota. The physical barrier includes the mucosal layer and epithelial layer, especially the tight junction and acidic pH of the gastric.[8] The main function of the physical barrier is to limit microbial access to tissue physically and biologically. The humoral component is antimicrobial peptides such as the β-defensins[9] and sIgA. Antimicrobial peptides have direct bactericidal activity, whereas sIgA acts by blocking the attachment of bacteria to epithelial cells, agglutination, or directly affecting bacterial virulence.
A cellular component is comprising a broad type of lymphoid and non-lymphoid cells. Non-lymphoid includes mucosal epithelial and M cells. Mucosal epithelial comprises a variety of cells with a specific function. Goblet cells, for example, responsible for producing mucus. Goblet cells abundantly present in the lower gastrointestinal tract and correlate with the mucosa layer's thickness.[10] Another unique cell in the mucosal area is M cells, which are crucial to transfer the antigen or pathogen from intestinal lumen to lamina propria, where other immune cells' recognition occurs. Therefore, many dendritic cells in the lamina propria side are ready to capture antigen or pathogen transferred by M cells. The dendritic cell will present the antigen to lymphocytes in the inductive site of mucosal immune site, where lymphocytes resident in the mucosal area. In the small intestine, the immune cell is relatively more heterogeneous compared to the colon. Here also exist intraepithelial lymphoid cells. It can directly release cytokine and killing the infected cells.[11]
One component of the mucosal immune system that does not belong to the human structure is commensal bacteria located in the mucosal area, but mostly in the gastrointestinal tract.[12] The commensal bacteria are able to protect our body by direct and indirect mechanism. The direct mechanism include nutrient competition, i.e., competition for sialic acid and fucose. Another direct mechanism is by releasing molecules that induce toxicity, i.e., bacteriocins. The indirect mechanism of protection involves metabolic production (i.e., bile salts and short-chain fatty acids) and the immune system's induction to release antibacterial molecule, i.e., defensins.[13]
Immune sensing
[edit | edit source]Cells in the innate immune system employ receptors to identify molecular structures formed by pathogens.[14] These receptors called as pathogen recognition receptors (PRRs), a class of germ line-encoded receptors, that recognize two classes of molecules: pathogen-associated molecular patterns (PAMPs) which frequently found in pathogens, and damage-associated molecular patterns (DAMPs), which released by damage or death cells.[15] Currently, known PRR families are the toll-like receptors (TLRs), the C-type lectin receptors (CLRs), the NOD–like receptors (NLRs), the RIG (retinoic acid-inducible gene)-like receptors (RLRs), and the AIM2-like receptor (ALR).[16] Toll-like receptors were first discovered in Drosophila, triggering the synthesis and secretion of cytokines, and activating other host defense programs required for both innate and adaptive immune responses. To date, 13 TLRs have been identified in mammals, of which 10 are present in humans (TLR1–10).[17]
Innate immune cells
[edit | edit source]The innate immune cells include the phagocyte (macrophages and neutrophils). The other cells involved in the innate response include innate lymphoid cells, natural killer cells), mast cells, eosinophils, and basophils. These cells identify and eliminate pathogens, either by attacking larger pathogens through contact or by engulfing and then killing microorganisms.[18]
Neutrophils and macrophages are phagocytes that travel throughout the body in pursuit of invading pathogens.[19] Neutrophils are normally found in the bloodstream and are the most abundant type of phagocyte, normally representing 50% to 60% of the total circulating leukocytes.[20] During the acute phase of inflammation, particularly as a result of bacterial infection, neutrophils is the first cells to arrive at the site of infection. Macrophages are versatile cells that reside within tissues and produce a wide array of chemicals including enzymes and cytokines, while they can also act as scavengers that eliminate dying cells and other debris, and as antigen-presenting cells that activate the adaptive immune system.[21]
Dendritic cells are located mainly in the skin, nose, lungs, stomach, and intestines. Dendritic cells serve as a link between the innate and adaptive immune systems, as they present antigens to T cells, one of the key cell types of the adaptive immune system.[22]
Granulocytes are caracterized by the presence of granules in their cytoplasm, that include mast cells, basophils, eosinophils, and neutrophils. Mast cells reside in connective tissues and mucous membranes, and regulate the inflammatory response.[23] Basophils and eosinophils are related to neutrophils. They secrete chemical mediators that are involved in defending against parasites and play a role in allergic reactions.[24]
Innate lymphoid cells (ILCs) are a group of innate immune system cells that are derived from common lymphoid progenitor and belong to the lymphoid lineage. These cells are defined by absence of antigen specific B cell receptor or T cell receptor (TCR) because of the lack of recombination activating gene. ILCs do not express myeloid or dendritic cell markers.[25]
Natural killer cells (NK cells), an ILCs, are lymphocytes and a component of the innate immune system which does not directly attack invading microbes.[26] Rather, NK cells destroy compromised host cells, such as tumor cells or virus-infected cells, recognizing such cells by a condition known as "missing self." This term describes cells with low levels of a cell-surface marker called MHC I (major histocompatibility complex)—a situation that can arise in viral infections of host cells.[27] Normal body cells are not recognized and attacked by NK cells because they express intact self MHC antigens. Those MHC antigens are recognized by killer cell immunoglobulin receptors which essentially put the brakes on NK cells.[28]
A minor subset of T cells, known as γδ T cells, can recognize intact antigens that are not bound to MHC receptors.[29][30]
Complement system
[edit | edit source]The complement system is a biochemical cascade that attacks the surfaces of foreign cells. It contains over 20 different proteins and is named for its ability to "complement" the killing of pathogens by antibodies. Complement is the major humoral component of the innate immune response.[31][32] The complement system can be activated through three major pathways: the classical pathway, the lectin pathway, and the alternative pathway. Each pathway is triggered by different stimuli, but all converge into a final common pathway that leads to the production of the same activated components, thus promoting inflammation and cell lysis.
Inflammatory response
[edit | edit source]
Inflammation is one of the first responses of the immune system to infection.[33] The symptoms of inflammation are redness, swelling, heat, and pain, which are caused by increased blood flow into tissue. Eicosanoids include prostaglandins that produce fever and the dilation of blood vessels associated with inflammation, and leukotrienes that attract certain white blood cells (leukocytes).[34][35] Common cytokines include interleukins that are responsible for communication between white blood cells; chemokines that promote chemotaxis; and interferons that have anti-viral effects, such as terminating protein synthesis in the host cell.[36] These cytokines and other chemicals recruit immune cells to the site of infection and promote healing of any damaged tissue following the removal of pathogens.[37]
The pattern-recognition receptors called inflammasomes are multiprotein complexes consisting of an NLR, the adaptor protein ASC, and the effector molecule pro-caspase-1. This structure forms in response to cytosolic PAMPs and DAMPs, whose function is to generate active forms of the inflammatory cytokines IL-1β and IL-18.[38]
Antiviral response
[edit | edit source]Upon viral infection, its genetic material that enters the cell will trigger the type I interferon production through the endosomal toll-like receptor or RIG-like receptor pathway.[39] Initially, this interferon is synthesized by infected cells and dendritic cells and is essential to inhibit viral replication. Further, natural killer cells will kill virus-infected cells before adaptive immunity response to fight the virus is developed. Several viruses can shut off MHC class I-antigen presentation, thus escaping recognition by cytotoxic T lymphocytes (CTL). Antibodies are effective against the virus only during the virus's extracellular stage, mainly by neutralizing the virus. The primary antibody contributing to this process is secretory IgA that neutralizes viral particles in the respiratory or intestinal mucosal. In the adaptive immune system, CTL is the main cell to eliminate virus infection. This cell recognized the endogenous viral peptide presented by MHC class I and directly showed its antiviral activity by killing the infected cells.
Adaptive immune system
[edit | edit source]
The adaptive immune system evolved in early vertebrates and allows for a stronger immune response as well as immunological memory, where each pathogen is "remembered" by a signature antigen.[40] The adaptive immune response is antigen-specific and requires the recognition of specific "non-self" antigens during a process called antigen presentation. Antigen specificity allows for the generation of responses that are tailored to specific pathogens or pathogen-infected cells. The ability to mount these tailored responses is maintained in the body by "memory cells". Should a pathogen infect the body more than once, these specific memory cells are used to quickly eliminate it.[41]
Adaptive immune cells
[edit | edit source]The main player in adaptive immune system is lymphocytes. B cells and T cells are the major types of lymphocytes and are derived from hematopoietic stem cells in the bone marrow.[27] The B cell antigen-specific receptor is an antibody molecule on the B cell surface and recognizes native (unprocessed) antigen without any need for antigen processing. Such antigens may be large molecules found on the surfaces of pathogens, but can also be small haptens (such as penicillin) attached to carrier molecule.[42] Each lineage of B cell expresses a different antibody, so the complete set of B cell antigen receptors represent all the antibodies that the body can manufacture.[27] When B or T cells encounter their related antigens they multiply and many "clones" of the cells are produced that target the same antigen.
Antigen presentation to T lymphocytes
[edit | edit source]Both B cells and T cells posses receptor molecules that recognize specific antigens. T cells recognize antigen, only after antigens have been processed into peptide and presented in combination with a major histocompatibility complex (MHC) molecule by APC.[43]
Cell mediated immunity
[edit | edit source]There are two major subtypes of T cells: the cytotoxic T cell and the T helper cell. In addition, there are regulatory T cells which have a role in modulating immune response.[44]
Cytotoxic T cells
[edit | edit source]Cytotoxic T cells are a sub-group of T cells that kill infected cells, as well as damaged or dysfunctional cells.[45] Cytotoxic T cells are activated when their T-cell receptor binds to the specific antigen in a complex with the MHC class I molecule of another cell. Recognition of this MHC:antigen complex is aided by a co-receptor on the T cell, called CD8. The T cell then travels throughout the body in search of cells where the MHC I receptors bear this antigen. When an activated T cell contacts such cells, it releases cytotoxins, such as perforin, which form pores in the target cell's plasma membrane, allowing ions, water, and toxins to enter. The entry of another toxin called ranulysin (a protease) induces the target cell to undergo apoptosis.[46] T cell killing of host cells is particularly important in preventing the replication of viruses. T cell activation is tightly controlled and generally requires a very strong MHC/antigen activation signal, or additional activation signals provided by "helper" T cells (see below).[46]
Helper T cells
[edit | edit source]Helper T cells regulate both the innate and adaptive immune responses and help determine which immune responses the body makes to a particular pathogen.[47][48] These cells have no cytotoxic activity and do not kill infected cells or clear pathogens directly. They instead control the immune response by directing other cells to perform these tasks.[49]
Helper T cells express T cell receptors that recognize antigen bound to Class II MHC molecules. The MHC:antigen complex is also recognized by the helper cell's CD4 co-receptor, which recruits molecules inside the T cell (such as Lck) that are responsible for the T cell's activation. Helper T cells have a weaker association with the MHC:antigen complex than observed for cytotoxic T cells, meaning many receptors on the helper T cell must be bound by an MHC:antigen to activate the helper cell, while killer T cells can be activated by engagement of a single MHC:antigen molecule. Helper T cell activation also requires longer duration of engagement with an antigen-presenting cell.[50] The activation of a resting helper T cell causes it to release cytokines that influence the activity of many cell types. Cytokine signals produced by helper T cells enhance the microbicidal function of macrophages and the activity of killer T cells.[51] In addition, helper T cell activation causes an upregulation of molecules expressed on the T cell's surface, such as CD40 ligand (also called CD154), which provide extra stimulatory signals typically required to activate antibody-producing B cells.[52]
Humoral immune response
[edit | edit source]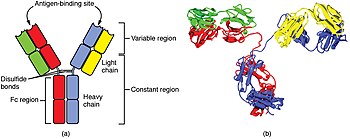
A B cell identifies pathogens when immunoglobulins on its surface bind to a specific foreign antigen.[54] This antigen/antibody complex is taken up by the B cell and processed by proteolysis into peptides. The B cell then displays these antigenic peptides on its surface MHC class II molecules. This combination of MHC and antigen attracts a matching helper T cell, which releases cytokine and activates the B cell.[55] Activated B cell then begins to divide and differentiate to plasma cells that secrete the antibody. These antibodies circulate in blood plasma and lymph, bind to pathogens expressing the antigen and mark them for destruction by complement activation or for uptake and destruction by phagocytes. Antibodies can also neutralize challenges directly, by binding to bacterial toxins or by interfering with the receptors that viruses and bacteria use to infect cells.[56]
Disorders of human immunity
[edit | edit source]Immunodeficiency
[edit | edit source]Immunodeficiency is the result of failure or lack of immune system components, including lymphocytes, phagocytes, and complement systems. These immunodeficiencies can be either primary (congenital), such as severe combined immunodeficiency (SCID), or secondary (acquired) as the one caused by HIV infection.[57]
Allergy
[edit | edit source]Allergy is a condition in which the body overreacts to exposure to a molecule. Allergy is type 1 hypersensitivity reactions mediated by activation of mast cells or basophils. This cellular activation results in the release of allergic mediators such as histamine and leukotrienes. These mediators play a role in clinical allergic responses, such as increased vascular permeability, bronchodilation, vasoconstriction, and the itch sensation. Mast cells can secrete histamine and other mediators after being activated by various types of molecules.
Autoimmunity
[edit | edit source]Overactive immune responses comprise the other end of immune dysfunction, particularly the autoimmune disorders. Here, the immune system fails to properly distinguish between self and non-self, and attacks part of the body. One of the functions of specialized cells (located in the thymus and bone marrow) is to present young lymphocytes with self antigens produced throughout the body and to eliminate those cells that recognize self-antigens, preventing autoimmunity.[54]
Manipulation in medicine
[edit | edit source]Immunosupression
[edit | edit source]Immunosuppressive drugs are used to control autoimmune disorders and prevent transplant rejection after an organ transplant.[58] Another drug class that often used for immunosuppresion is glucocorticoid. Glucocorticoid have antiinflammatory and immunosuppresive property[59]and often used in conjunction with cytotoxic or immunosuppressive in low doses. Cytotoxic such as azathioprine inhibit the immune response by killing dividing cells such as activated T cells. However, the killing is indiscriminate and other constantly dividing cells and their organs are affected, which causes toxic side effects.[58] Immunosuppressive drugs such as cyclosporin prevent T cells from responding to signals correctly by inhibiting signal transduction pathways.[60]
Vaccination
[edit | edit source]Long-term active memory is acquired following infection by activation of B and T cells. Active immunity can also be generated artificially through vaccination. Vaccination is based on the introduction of an antigen from a pathogen in order to stimulate the immune system and develop an adaptive immune response against that specific pathogen without triggering the associated disease.[61] This deliberate induction of an immune response is effective because it harnesses the natural specificity and inducibility of the immune system. Vaccination is the most effective manipulation of the immune system that humans have developed, given that infectious disease remains one of the top causes of death in the population.[62]
Most viral vaccines are based on live attenuated viruses, whereas many bacterial vaccines are based on acellular components of micro-organisms, including harmless toxin components.[61] Since many antigens derived from acellular vaccines do not strongly induce the adaptive response, most bacterial vaccines are provided with additional adjuvants that activate the antigen-presenting cells and maximize immunogenicity.[63]
Tumor immunology
[edit | edit source]The immune system responds not only to pathogens but also to transformed cells. In the 1950s, Macfarlane Burnet proposed the cancer immune surveillance concept, that the immune system is able to identify and destroy transformed cell clones and to kill the cancer cells that have formed.[64] Cancer immunosurveillance appears to be an important host protection mechanism that reduces cancer rates by inhibiting carcinogenesis and maintaining normal cellular homeostasis.[65] The transformed cells express antigens encoded by mutated genes (neoantigens) that are absent on normal cells. Mostly, the neoantigens are the products of randomly mutated genes that are not involved in carcinogenesis, or less commonly, products of mutated genes involved in oncogenesis. Consequently, new MHC-binding peptides are generated and provoke adaptive immune system mediated by T cells. Some antigens are derived from oncogenic viruses such as human papillomavirus (HPV), which causes carcinoma of the uterine cervical, mouth, and throat. In addition, some tumor antigens are the products made by normal cells but produced in excessive amounts by tumors, since the genes that encode these proteins are amplified. For instance, one type of epidermal growth factor called Her2 is overexpressed in some breast cancers. Therefore, the trastuzumab monoclonal antibody against Her2 is used to treat patients whose tumors display a high expression of Her2.
Additional information
[edit | edit source]Acknowledgements
[edit | edit source]Any people, organisations, or funding sources that you would like to thank.
Competing interests
[edit | edit source]None.
Ethics statement
[edit | edit source]No animal or human was involved as research subject.
References
[edit | edit source]- ↑ Donnenberg, Michael S. (2000-08). "Pathogenic strategies of enteric bacteria". Nature 406 (6797): 768–774. doi:10.1038/35021212. http://www.nature.com/articles/35021212.
- ↑ Riera Romo, Mario; Pérez-Martínez, Dayana; Castillo Ferrer, Camila (2016-06). "Innate immunity in vertebrates: an overview". Immunology 148 (2): 125–139. doi:10.1111/imm.12597. PMID 26878338. PMC PMC4863567. http://doi.wiley.com/10.1111/imm.12597.
- ↑ Restifo, Nicholas P; Gattinoni, Luca (2013-10). "Lineage relationship of effector and memory T cells". Current Opinion in Immunology 25 (5): 556–563. doi:10.1016/j.coi.2013.09.003. PMID 24148236. PMC PMC3858177. https://linkinghub.elsevier.com/retrieve/pii/S0952791513001386.
- ↑ Kurosaki, Tomohiro; Kometani, Kohei; Ise, Wataru (2015-03). "Memory B cells". Nature Reviews Immunology 15 (3): 149–159. doi:10.1038/nri3802. http://www.nature.com/articles/nri3802.
- ↑ Medzhitov, Ruslan (2007-10-18). "Recognition of microorganisms and activation of the immune response". Nature 449 (7164): 819–826. doi:10.1038/nature06246. PMID 17943118. https://www.ncbi.nlm.nih.gov/pubmed/17943118.
- ↑ Matzinger, Polly (2002-04-12). "The danger model: a renewed sense of self". Science (New York, N.Y.) 296 (5566): 301–305. doi:10.1126/science.1071059. PMID 11951032. https://www.ncbi.nlm.nih.gov/pubmed/11951032.
- ↑ McGhee, Jerry R.; Fujihashi, Kohtaro (2012). "Inside the Mucosal Immune System". PLoS Biology 10 (9): e1001397. doi:10.1371/journal.pbio.1001397. PMID 23049482. PMC PMC3457930. https://dx.plos.org/10.1371/journal.pbio.1001397.
- ↑ Smith, James L. (2003-07-01). "The Role of Gastric Acid in Preventing Foodborne Disease and How Bacteria Overcome Acid Conditions†". Journal of Food Protection 66 (7): 1292–1303. doi:10.4315/0362-028X-66.7.1292. https://meridian.allenpress.com/jfp/article/66/7/1292/168120/The-Role-of-Gastric-Acid-in-Preventing-Foodborne.
- ↑ Agerberth, B.; Gudmundsson, G. H. (2006). "Host antimicrobial defence peptides in human disease". Current Topics in Microbiology and Immunology 306: 67–90. ISSN 0070-217X. PMID 16909918. https://www.ncbi.nlm.nih.gov/pubmed/16909918.
- ↑ Rogers, Duncan F (2003). "The airway goblet cell". The International Journal of Biochemistry & Cell Biology 35 (1): 1–6. doi:10.1016/S1357-2725(02)00083-3. https://linkinghub.elsevier.com/retrieve/pii/S1357272502000833.
- ↑ Varol, Chen; Vallon-Eberhard, Alexandra; Elinav, Eran; Aychek, Tegest; Shapira, Yami; Luche, Hervé; Fehling, Hans Jörg; Hardt, Wolf-Dietrich et al. (2009). "Intestinal Lamina Propria Dendritic Cell Subsets Have Different Origin and Functions". Immunity 31 (3): 502–512. doi:10.1016/j.immuni.2009.06.025. ISSN 1074-7613. https://linkinghub.elsevier.com/retrieve/pii/S1074761309003628.
- ↑ Thursby, Elizabeth; Juge, Nathalie (2017). "Introduction to the human gut microbiota". Biochemical Journal 474 (11): 1823–1836. doi:10.1042/BCJ20160510. PMID 28512250. PMC PMC5433529. https://portlandpress.com/biochemj/article/474/11/1823/49429/Introduction-to-the-human-gut-microbiota.
- ↑ Macpherson, Andrew J.; Geuking, Markus B.; McCoy, Kathy D. (2005). "Immune responses that adapt the intestinal mucosa to commensal intestinal bacteria". Immunology 115 (2): 153–162. doi:10.1111/j.1365-2567.2005.02159.x. ISSN 0019-2805. PMID 15885120. PMC PMC1782138. http://doi.wiley.com/10.1111/j.1365-2567.2005.02159.x.
- ↑ Kumar, Himanshu; Kawai, Taro; Akira, Shizuo (2011). "Pathogen Recognition by the Innate Immune System". International Reviews of Immunology 30 (1): 16–34. doi:10.3109/08830185.2010.529976. http://www.tandfonline.com/doi/full/10.3109/08830185.2010.529976.
- ↑ Amarante-Mendes, Gustavo P.; Adjemian, Sandy; Branco, Laura Migliari; Zanetti, Larissa C.; Weinlich, Ricardo; Bortoluci, Karina R. (2018). "Pattern Recognition Receptors and the Host Cell Death Molecular Machinery". Frontiers in Immunology 9: 2379. doi:10.3389/fimmu.2018.02379. PMID 30459758. PMC PMC6232773. https://www.frontiersin.org/article/10.3389/fimmu.2018.02379/full.
- ↑ Jang, Ji-Hyun; Shin, Hee Woong; Lee, Jung Min; Lee, Hyeon-Woo; Kim, Eun-Cheol; Park, Sang Hyuk (2015). "An Overview of Pathogen Recognition Receptors for Innate Immunity in Dental Pulp". Mediators of Inflammation 2015: 1–12. doi:10.1155/2015/794143. PMID 26576076. PMC PMC4630409. http://www.hindawi.com/journals/mi/2015/794143/.
- ↑ Vijay, Kumar (2018). "Toll-like receptors in immunity and inflammatory diseases: Past, present, and future". International Immunopharmacology 59: 391–412. doi:10.1016/j.intimp.2018.03.002. PMID 29730580. PMC PMC7106078. https://linkinghub.elsevier.com/retrieve/pii/S156757691830095X.
- ↑ Murphy, Kenneth (2017). Janeway's immunobiology. Weaver, Casey (Ninth ed.). New York, NY, USA: Garland Science. ISBN 9780815345053. OCLC 933586700. https://www.worldcat.org/oclc/933586700.
- ↑ Zen, Ke; Parkos, Charles A. (2003-10). "Leukocyte-epithelial interactions". Current Opinion in Cell Biology 15 (5): 557–564. ISSN 0955-0674. PMID 14519390. https://www.ncbi.nlm.nih.gov/pubmed/14519390.
- ↑ Stvrtinová, Viera; Jakubovský, Ján; Hulín, Ivan (1995). Inflammation and Fever from Pathophysiology: Principles of Disease. Computing Centre, Slovak Academy of Sciences: Academic Electronic Press. ISBN 80-967366-1-2. Archived from the original on 11 July 2001. https://web.archive.org/web/20010711220523/http://nic.savba.sk/logos/books/scientific/Inffever.html. Retrieved 1 January 2007.
- ↑ Rua, Rejane; McGavern, Dorian B. (2015-9). "Elucidation of monocyte/macrophage dynamics and function by intravital imaging". Journal of Leukocyte Biology 98 (3): 319–332. doi:10.1189/jlb.4RI0115-006RR. ISSN 1938-3673. PMID 26162402. PMC PMC4763596. https://www.ncbi.nlm.nih.gov/pubmed/26162402.
- ↑ Guermonprez, Pierre; Valladeau, Jenny; Zitvogel, Laurence; Théry, Clotilde; Amigorena, Sebastian (2002). "Antigen presentation and T cell stimulation by dendritic cells". Annual Review of Immunology 20: 621–667. doi:10.1146/annurev.immunol.20.100301.064828. ISSN 0732-0582. PMID 11861614. https://www.ncbi.nlm.nih.gov/pubmed/11861614.
- ↑ Krishnaswamy, Guha; Ajitawi, Omar; Chi, David S. (2006). "The human mast cell: an overview". Methods in Molecular Biology (Clifton, N.J.) 315: 13–34. ISSN 1064-3745. PMID 16110146. https://www.ncbi.nlm.nih.gov/pubmed/16110146.
- ↑ Kariyawasam, Harsha H.; Robinson, Douglas S. (2006-4). "The eosinophil: the cell and its weapons, the cytokines, its locations". Seminars in Respiratory and Critical Care Medicine 27 (2): 117–127. doi:10.1055/s-2006-939514. ISSN 1069-3424. PMID 16612762. https://www.ncbi.nlm.nih.gov/pubmed/16612762.
- ↑ "Innate lymphoid cells: emerging insights in development, lineage relationships, and function". Annual Review of Immunology 30: 647–75. 2012. doi:10.1146/annurev-immunol-020711-075053. PMID 22224763.
- ↑ Gabrielli, Sara; Ortolani, Claudio; Del Zotto, Genny; Luchetti, Francesca; Canonico, Barbara; Buccella, Flavia; Artico, Marco; Papa, Stefano et al. (2016). "The Memories of NK Cells: Innate-Adaptive Immune Intrinsic Crosstalk". Journal of Immunology Research 2016: 1376595. doi:10.1155/2016/1376595. ISSN 2314-7156. PMID 28078307. PMC PMC5204097. https://www.ncbi.nlm.nih.gov/pubmed/28078307.
- ↑ 27.0 27.1 27.2 Janeway 2005.
- ↑ Rajalingam 2012, Chapter: Overview of the killer cell immunoglobulin-like receptor system.
- ↑ "gammadelta T cells link innate and adaptive immune responses". Chemical Immunology and Allergy 86: 151–83. 2005. doi:10.1159/000086659. ISBN 3-8055-7862-8. PMID 15976493.
- ↑ "Iodine, thymus, and immunity". Nutrition 25 (9): 977–79. September 2009. doi:10.1016/j.nut.2009.06.002. PMID 19647627.
- ↑ Rus, Horea; Cudrici, Cornelia; Niculescu, Florin (2005). "The role of the complement system in innate immunity". Immunologic Research 33 (2): 103–112. doi:10.1385/IR:33:2:103. ISSN 0257-277X. PMID 16234578. https://www.ncbi.nlm.nih.gov/pubmed/16234578.
- ↑ Degn, S. E.; Thiel, S. (2013-8). "Humoral pattern recognition and the complement system". Scandinavian Journal of Immunology 78 (2): 181–193. doi:10.1111/sji.12070. ISSN 1365-3083. PMID 23672641. https://www.ncbi.nlm.nih.gov/pubmed/23672641.
- ↑ Kawai, Taro; Akira, Shizuo (2006-2). "Innate immune recognition of viral infection". Nature Immunology 7 (2): 131–137. doi:10.1038/ni1303. ISSN 1529-2908. PMID 16424890. https://www.ncbi.nlm.nih.gov/pubmed/16424890.
- ↑ Miller, Stephen B. (2006-8). "Prostaglandins in health and disease: an overview". Seminars in Arthritis and Rheumatism 36 (1): 37–49. doi:10.1016/j.semarthrit.2006.03.005. ISSN 0049-0172. PMID 16887467. https://www.ncbi.nlm.nih.gov/pubmed/16887467.
- ↑ Ogawa, Yoshiko; Calhoun, William J. (2006-10). "The role of leukotrienes in airway inflammation". The Journal of Allergy and Clinical Immunology 118 (4): 789–798; quiz 799–800. doi:10.1016/j.jaci.2006.08.009. ISSN 0091-6749. PMID 17030228. https://www.ncbi.nlm.nih.gov/pubmed/17030228.
- ↑ Le, Yingying; Zhou, Ye; Iribarren, Pablo; Wang, Jiming (2004-4). "Chemokines and chemokine receptors: their manifold roles in homeostasis and disease". Cellular & Molecular Immunology 1 (2): 95–104. ISSN 1672-7681. PMID 16212895. https://www.ncbi.nlm.nih.gov/pubmed/16212895.
- ↑ Martin, Paul; Leibovich, S. Joseph (2005-11). "Inflammatory cells during wound repair: the good, the bad and the ugly". Trends in Cell Biology 15 (11): 599–607. doi:10.1016/j.tcb.2005.09.002. ISSN 0962-8924. PMID 16202600. https://www.ncbi.nlm.nih.gov/pubmed/16202600.
- ↑ "NOD-like receptors and inflammasomes: A review of their canonical and non-canonical signaling pathways". Archives of Biochemistry and Biophysics 670: 4–14. February 2019. doi:10.1016/j.abb.2019.02.008. PMID 30772258.
- ↑ Lester, Sandra N.; Li, Kui (2014). "Toll-Like Receptors in Antiviral Innate Immunity". Journal of Molecular Biology 426 (6): 1246–1264. doi:10.1016/j.jmb.2013.11.024. PMID 24316048. PMC PMC3943763. https://linkinghub.elsevier.com/retrieve/pii/S0022283613007353.
- ↑ "The evolution of adaptive immunity". Annual Review of Immunology 24 (1): 497–518. 2006. doi:10.1146/annurev.immunol.24.021605.090542. PMID 16551257.
- ↑ Sompayrac 2019, p. 38.
- ↑ Janeway, Travers & Walport 2001, sec. 12-10.
- ↑ Sompayrac 2019, pp. 51–53.
- ↑ Sompayrac 2019, pp. 7–8.
- ↑ "CD8+ T cell effector mechanisms in resistance to infection". Annual Review of Immunology 18 (1): 275–308. 2000. doi:10.1146/annurev.immunol.18.1.275. PMID 10837060.
- ↑ 46.0 46.1 "T-cell receptor signaling events triggering granule exocytosis". Critical Reviews in Immunology 26 (3): 265–90. 2006. doi:10.1615/CritRevImmunol.v26.i3.40. PMID 16928189.
- ↑ "Functional diversity of helper T lymphocytes". Nature 383 (6603): 787–93. Oct 1996. doi:10.1038/383787a0. PMID 8893001.
- ↑ "Helper T cell-regulated B cell immunity". Current Topics in Microbiology and Immunology 311: 59–83. 2006. doi:10.1007/3-540-32636-7_3. ISBN 978-3-540-32635-9. PMID 17048705.
- ↑ Sompayrac 2019, p. 8.
- ↑ "Human CD8+ T cells do not require the polarization of lipid rafts for activation and proliferation". Proceedings of the National Academy of Sciences of the United States of America 99 (23): 15006–11. Nov 2002. doi:10.1073/pnas.232058599. PMID 12419850. PMC 137535. //www.ncbi.nlm.nih.gov/pmc/articles/PMC137535/.
- ↑ Alberts et al. 2002, Chapter. "Helper T Cells and Lymphocyte Activation".
- ↑ "CD40 and CD154 in cell-mediated immunity". Annual Review of Immunology 16 (1): 111–35. 1998. doi:10.1146/annurev.immunol.16.1.111. PMID 9597126.
- ↑ "Understanding the Immune System: How it Works" (PDF). National Institute of Allergy and Infectious Diseases (NIAID). Archived from the original (PDF) on 3 January 2007. Retrieved 1 January 2007.
- ↑ 54.0 54.1 Sproul, T. W.; Cheng, P. C.; Dykstra, M. L.; Pierce, S. K. (2000). "A role for MHC class II antigen processing in B cell development". International Reviews of Immunology 19 (2-3): 139–155. ISSN 0883-0185. PMID 10763706. https://www.ncbi.nlm.nih.gov/pubmed/10763706.
- ↑ Parker, D. C. (1993). "T cell-dependent B cell activation". Annual Review of Immunology 11: 331–360. doi:10.1146/annurev.iy.11.040193.001555. ISSN 0732-0582. PMID 8476565. https://www.ncbi.nlm.nih.gov/pubmed/8476565.
- ↑ Forthal, Donald N. (2014-08-15). "Functions of Antibodies". Microbiology Spectrum 2 (4): 1–17. ISSN 2165-0497. PMID 25215264. PMC PMC4159104. https://www.ncbi.nlm.nih.gov/pubmed/25215264.
- ↑ Notarangelo, Luigi D.; Fischer, Alain; Geha, Raif S.; Casanova, Jean-Laurent; Chapel, Helen; Conley, Mary Ellen; Cunningham-Rundles, Charlotte; Etzioni, Amos et al. (2009). "Primary immunodeficiencies: 2009 update". Journal of Allergy and Clinical Immunology 124 (6): 1161–1178. doi:10.1016/j.jaci.2009.10.013. PMID 20004777. PMC PMC2797319. https://linkinghub.elsevier.com/retrieve/pii/S0091674909015401.
- ↑ 58.0 58.1 Taylor, Anna L.; Watson, Christopher J. E.; Bradley, J. Andrew (2005-10). "Immunosuppressive agents in solid organ transplantation: Mechanisms of action and therapeutic efficacy". Critical Reviews in Oncology/Hematology 56 (1): 23–46. doi:10.1016/j.critrevonc.2005.03.012. ISSN 1040-8428. PMID 16039869. https://www.ncbi.nlm.nih.gov/pubmed/16039869.
- ↑ Barnes, Peter J. (2006-03-08). "Corticosteroids: the drugs to beat". European Journal of Pharmacology 533 (1-3): 2–14. doi:10.1016/j.ejphar.2005.12.052. ISSN 0014-2999. PMID 16436275. https://www.ncbi.nlm.nih.gov/pubmed/16436275.
- ↑ Masri, Marwan A. (2003-7). "The mosaic of immunosuppressive drugs". Molecular Immunology 39 (17-18): 1073–1077. ISSN 0161-5890. PMID 12835079. https://www.ncbi.nlm.nih.gov/pubmed/12835079.
- ↑ 61.0 61.1 Cite error: Invalid
<ref>tag; no text was provided for refs namedAlberts - ↑ Pulendran, Bali; Ahmed, Rafi (2011-6). "Immunological mechanisms of vaccination". Nature Immunology 12 (6): 509–517. ISSN 1529-2916. PMID 21739679. PMC PMC3253344. https://www.ncbi.nlm.nih.gov/pubmed/21739679.
- ↑ Singh, M.; O'Hagan, D. (1999-11). "Advances in vaccine adjuvants". Nature Biotechnology 17 (11): 1075–1081. doi:10.1038/15058. ISSN 1087-0156. PMID 10545912. https://www.ncbi.nlm.nih.gov/pubmed/10545912.
- ↑ Dunn, Gavin P.; Bruce, Allen T.; Ikeda, Hiroaki; Old, Lloyd J.; Schreiber, Robert D. (2002). "Cancer immunoediting: from immunosurveillance to tumor escape". Nature Immunology 3 (11): 991–998. doi:10.1038/ni1102-991. ISSN 1529-2908. http://www.nature.com/articles/ni1102-991.
- ↑ Kim, Ryungsa; Emi, Manabu; Tanabe, Kazuaki (2007). "Cancer immunoediting from immune surveillance to immune escape". Immunology 121 (1): 1–14. doi:10.1111/j.1365-2567.2007.02587.x. PMID 17386080. PMC PMC2265921. http://doi.wiley.com/10.1111/j.1365-2567.2007.02587.x.

