Motivation and emotion/Book/2019/Psychological flexibility and emotional health
What is psychological flexibility and what role does it play in emotional health?
Overview
[edit | edit source]Mental health is being talked about more and more these days and there is extensive psychological research on all aspects of this issue. Psychological flexibility and emotional health play a large part in mental illness and our overall health (Sandoz, Moyer & Armelie, 2015). In this book chapter, aspects of psychological flexibility and emotional health are discussed and methods of improving them are proposed.
|
What is psychological flexibility and why is it important?
[edit | edit source]Psychological flexibility or resiliency is a broad term and involves many psychological mechanisms and skills. It includes tolerance, the ability to cope and recover from difficult times, accepting change and open communication skills. High psychological flexibility means you are able to experience the present moment and everyday life even when you are in a very difficult situation or emotional state. Therapies that aim to improve psychological flexibility appear to improve things like job stress, a wide range mental health disorders, low emotional health and lack of coping mechanisms, and reduce self-harm (Sandoz, Moyer & Armelie, 2015).
|
Psychological flexibility is a very important factor interpersonal relationships, mental health and dealing with trauma (Sandoz, Moyer & Armelie, 2015). |
Psychological flexibility is important in romantic relationships. Couples with higher flexibility and emotional acceptance tend to have higher relationship satisfaction, and this applies to couples in distress and not in distress with their relationships (Sandoz, Moyer & Armelie, 2015). Psychological flexibility is also important for partners to support each other through hardship (Köhle et al., 2017). Psychological flexibility is also a major factor in the relationship between parents and children. There's a relationship between lower psychological flexibility and parental depression and parenting stress, which as a result makes parents more likely to have inconsistent and incoherent parenting behaviour and emphasise punishment. It can also make parents controlling, and this can all increase anxiety in children. Improving flexibility in families and marriages is a major intervention target, as well as parental stress management (Sandoz, Moyer & Armelie, 2015; Whittingham, Sanders, McKinlay & Boyd, 2013). Psychological flexibility also plays a significant part in both developing and recovering from trauma or Post-traumatic stress disorder (PTSD). Struggling to cope with, recover from and accept difficult emotions, thoughts, sensations or memories predicts longer-term PTSD and other trauma related disorders and worsens quality of life. While others with higher psychological flexibility are more likely to grow after their traumatic experience and find meaning in their life again (Meyer et al., 2018; Reid et al., 2017; Sandoz, Moyer & Armelie, 2015). Managing change is also a challenge to people. Change is a part of life and major life changes happen multiple times throughout our lives. Coping with change is an indicator of good psychological flexibility (Sandoz, Moyer & Armelie, 2015).
|
Quiz 1
|
What is emotional health?
[edit | edit source]Emotional health regards to how well an individual can manage and express their wide mix of emotions (see Figure 1). Struggles with regulating emotions tend to lead to poorer psychological outcomes and as a result more mental health problems (Spidel, Lecomte, Kealy & Daigneault, 2017). Finding it difficult to identify and describe your feelings tends to lead to poorer emotional adjustment (Landstra, Ciarrochi, Deane & Hillman, 2013). Emotional dysregulation is commonly a target for treatment of psychological disorders, from common depression and anxiety disorders (Burckhardt, Manicavasagar, Batterham, Hadzi-Pavlovic & Shand, 2017) to Borderline Personality Disorder (BPD) and Substance Use Disorders (SUD) (Hall et al., 2018; Montgomery, Kim & Franklin, 2011).
Neurological mechanisms of emotions
[edit | edit source]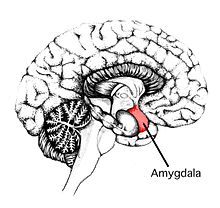
The neurological mechanisms of emotions seem to be something that's not thought of often, because it all seems just psychological. When really, emotions are necessary and evolutionary functions in humans and knowing what happens in the brain with emotions is really important (see Figure 2). The brain can detect emotional threats with emotional threat detection circuits (Gilam and Hendler, 2015). The brain also has emotional regulation and emotional awareness circuits (Deak, 2011; Gilam and Hendler, 2015), as well as reward circuits (Pariyagath, Gowin and Stein (2015). The periaqueductal grey plays a major role in both motivation and emotion. It works with the amygdala (see Figure 3) in decision-making. Hormone drives, which influence emotions, come from the hypothalamus (Blair, 2012).
How do psychological flexibility and emotional health affect each another?
[edit | edit source]Research shows the level of an individual's psychological flexibility has an impact on emotional health and regulation, and lower emotional health impairs psychological flexibility. The two play into each other a great amount and they both play a major role in your well-being (George & de Guzman, 2015; Sandoz, Moyer & Armelie, 2015; Spidel, Lecomte, Kealy & Daigneault, 2017). Support and coherence from family, friends and partners are all crucial for upholding psychological flexibility and emotional health (Sandoz, Moyer & Armelie, 2015).

Mental illness
[edit | edit source]Extensive research on the implications of high or low psychological flexibility and emotion regulation show clear links to psychological disorders, both in developing them and treating them (Reid et al., 2017; Sandoz, Moyer & Armelie, 2015). Treatment to improve emotion regulation is very beneficial for individuals with psychosis, a history of trauma, depression, anxiety disorders (see Figure 4), BPD and substance abuse (Burckhardt, Manicavasagar, Batterham, Hadzi-Pavlovic & Shand, 2017; Hall et al., 2018; Montgomery, Kim & Franklin, 2011; Spidel, Lecomte, Kealy & Daigneault, 2017). Willingness to be exposed to unpleasant experiences has been seen as a predictor for successful exposure therapy for obsessive-compulsive disorder. This means exercising psychological flexibility can lead to better mental health outcomes (Reid et al., 2017).
Touching on mental health stigma, some interesting research found a link between lower psychological flexibility and stigmatizing individuals with mental health disorders. So not only is stigma damaging to those with mental health disorders, it also leads to or results from poorer psychological outcomes in the stigmatizer (Masuda, Price, Anderson, Schmertz & Calamaras, 2009).
Burnout
[edit | edit source]Burnout refers to exhaustion from over-working and is related to low self-esteem, job difficulties, dropouts, suicidal thoughts and self-harm. Problems with burnout are becoming more common and serious nowadays, particularly in students and those working in the health profession. It's an issue that educational institutions and workplaces need to be more aware of. Research shows higher levels of psychological flexibility may lead to lower levels of burnout as people are more able to cope with the demands and can focus on the present goals. This suggests developing skills to increase psychological flexibility would in turn reduce the likelihood of suffering from burnout or at least dealing with it more effectively (Robins, Roberts & Sarris, 2015)
How can people improve and manage their psychological flexibility and emotional health?
[edit | edit source]There is help for people struggling to cope with their emotions or get through very difficult periods of their life, and it doesn't all need to be in a clinical setting which may not be accessible to everyone.
Acceptance and Commitment Therapy
[edit | edit source]Acceptance and Commitment Therapy (ACT) has been backed up by research as being an effective and reliable treatment to help with psychological distress and emotion regulation. This is widely applicable to psychological disorders, people facing hardship and introducing and adapting to lifestyle and thinking style changes (Köhle et al., 2017; Montgomery, Kim & Franklin, 2011; Sahebari, Asghari Ebrahimabad, Shoraketokanlo, Aghamohammadian Sharbaf & Khodashahi, 2019; Sairanen et al., 2017). Incorporating this with mindfulness is even more effective (George & de Guzman, 2015). Acceptance and Commitment therapy to help with symptoms related to psychosis and a history of trauma has also shown to be promising, and also seems to increase adherence to treatment (Spidel, Lecomte, Kealy & Daigneault, 2017).
|
There are six main skills that ACT tries to instill (see Table 1), which promote mindfulness and acceptance and result in an increase in psychological flexibility. They are: acceptance, cognitive diffusion, contact with the present moment, self as context, values and committed action (Gutierrez & Hagedorn, 2013; Hayes et al, 2006). |
Table 1.
Six main skills of ACT
| Skill | Explanation |
|---|---|
| Acceptance | Acceptance techniques are for improving skills for countering avoidance and rather accepting and staying present with their memories, thoughts, and feelings, without the intensity and frequency (Gutierrez & Hagedorn, 2013; (Gutierrez & Hagedorn, 2013; Hayes et al, 2006).). |
| Cognitive diffusion | This is a significant part of ACT. Cognitive diffusion involves using new ways to respond to thoughts by realising of the context of the thought and it's negative implications. For example, someone thinking they are hopeless and horrible can start to realise through cognitive diffusion that these are just thoughts - a mental process - and not a true reflection of themselves. This helps to alleviate negative feelings and behaviours from those thoughts. Some techniques are thanking the mind for a thought or just observing it, labelling thoughts as just stories (such as "it's just the terrible me story going on in my head again"), or repeating negative thoughts or words until it loses its negative connotation. This technique doesn't remove these thoughts, it just helps to reduce attachment and emotional reactions to thoughts, and that thoughts are just thoughts (Gutierrez & Hagedorn, 2013; Hayes et al, 2006). |
| Contact with present moment | Contact with the present moment refers to objective and non-judgmental awareness of both the mind and the surrounding physical environment. This is important because this helps to become more in the present moment, instead of focusing on their negative and unhelpful thoughts, feelings and memories (Gutierrez & Hagedorn, 2013; Hayes et al, 2006). |
| Self as context | Self as context or observing the self involves a perception of the self as universal and not part of personal experiences and behaviours. It means essentially noticing everything that is going on around you and becoming aware that you exist separate from your experiences and behaviours. This helps to identify personal values, as well as simply being aware of their experiences instead of becoming attached to experiences (Gutierrez & Hagedorn, 2013; Hayes et al, 2006). |
| Values | Values shape your directions and attitudes in life and they are reflected in present moments. They help to inform a committed action (Gutierrez & Hagedorn, 2013; Hayes et al, 2006). |
| Committed action | After identifying your values, you can apply these to every day life and your future plans, which is called committed action. Setting goals is a part of committed action (see Figure 5) and having a set goal can help improve your motivation (see Figure 6). Barriers such as shame or avoidance can be countered by reminding yourself of your values (Gutierrez & Hagedorn, 2013; Hayes et al, 2006). |
A study (Harvey et al., n.d.) showed ACT was beneficial for soldiers struggling with anger problems, alcohol use and stress issues. During post-treatment the soldiers had significant reductions in anger, aggression, stress and anxiety, alcohol use and perceptions of other people being at fault for their problems. These results clearly show that through ACT they were able to develop their self-awareness and better manage their emotions. ACT has also been effective for people suffering from chronic pain, enabling with the right coping skills (Nes, van Dulmen, Wicksell, Fors & Eide, 2017). ACT has also been used for managing parental stress management (Whittingham, Sanders, McKinlay & Boyd, 2013), aiding interpersonal relationships get through difficult periods (Köhle et al., 2017) as well as weight loss and eating habits. ACT enhances a person's capacity to follow through with things they strive for even if it brings up negative emotions (Sairanen et al., 2017). ACT also provides help for repetitive negative thinking (RNT) (Ruiz, Riaño Hernández, Suárez Falcón & Luciano, 2016). RNT is excessive worry and rumination in the face of distress and understandably plays a role in the development and recovery of psychological disorders. A study by Ruiz, Riaño Hernández, Suárez Falcón & Luciano, 2016 implemented one session of ACT for people struggling with RNT, with the people using a self-register everyday. During the 6-week follow-up, the wide majority of them had significant reductions in pathological worry, rumination and frequency of their negative thoughts. Another study (Burckhardt, Manicavasagar, Batterham, Hadzi-Pavlovic & Shand, 2017) found ACT to be a potential preventative measure against anxiety and depression in adolescents, and proposed the intervention was feasible to implement in schools. So ACT is something that could be used in a casual setting. This is also an opportunity for psychoeducation (Cartwright & Hooper, 2017). Overall, ACT is a very promising area for treating anxiety disorders, depression, psychosis, epilepsy and other various mental or physiological disorders. It provides a different approach to facing difficult situations and illnesses (Montgomery, Kim & Franklin, 2011). Mindfulness-based self-efficacy can be developed with ACT along with psychological flexibility (Cartwright & Hooper, 2017).
Rational emotive behaviour therapy
[edit | edit source]Rational emotive behaviour therapy (REBT) is also a psychological therapy that helps people to learn to respond to their emotions and challenges differently. During REBT, people learn about the interactions between their thoughts, behaviours and emotions, which provides a form of psychoeducation. During REBT people also learn self-acceptance and how to become self-sufficient. REBT is based on ABC theory, which suggests that people have an emotional response off activating events, which is what the "A" stands for in ABC. The strength and direction of the emotional response is defined by the person's thoughts about the event, and the difficulties come from self-disturbing beliefs, which is "B". This is what results in the emotional consequence, which is "C". REBT is dependent on the client identifying whether their thoughts and beliefs are rational or irrational, Changing irrational thoughts can have major effects on our emotions and our behaviour (Ellis & Joffe Ellis, 2011; Rait, Monsen, & Squires, 2010).
Other therapies and techniques
[edit | edit source]Other psychological therapies or techniques to improve psychological flexibility and emotional health are cognitive behaviour therapy (CBT) and meditation and mindfulness techniques. Mindfulness-based cognitive therapy (MBCT) has become a popular type of cognitive therapy, which focuses more on mindfulness than traditional CBT (Fledderus, Bohlmeijer, Smit & Westerhof, 2010; George & de Guzman, 2015).
Physical activity and nature
[edit | edit source]Research shows physical activity and being in the outdoors can have significant positive effects on our emotional well-being, as well as of course our physical health. Being in nature specifically adds extra positive effects (Nes, van Dulmen, Wicksell, Fors & Eide, 2017; Pasanen, Tyrväinen & Korpela, 2014). Physical activity also adds an outlet to your life and you can make it into something fun (see Figure 7).

|
Quiz 2
|
Conclusion
[edit | edit source]Psychological flexibility is essentially how well we respond and cope with difficult situations that we face. Dealing with change, tolerating strong emotions and open communication are all predicative of psychological flexibility. Being able to be in the present moment while dealing with emotional distress and hardship is also a key element of psychological flexibility, and this is often a difficult task for us all. Having low psychological flexibility, meaning not having the capacity to cope with negative situations and feelings, inevitably leads to poorer emotional health (Sandoz, Moyer & Armelie, 2015; Spidel, Lecomte, Kealy & Daigneault, 2017). It lets these situations take a toll on us. Thankfully there are ways to get help to improve psychological flexibility and in turn your emotional health. ACT is backed up by a lot of research to be very effective for everything from general stress and negative thinking, to psychological disorders like anxiety or borderline personality disorder, to helping to cope with physiological health problems like cancer (Burckhardt, Manicavasagar, Batterham, Hadzi-Pavlovic & Shand, 2017; Hall et al., 2018; Harvey et al., n.d.; Montgomery, Kim & Franklin, 2011; Ruiz, Riaño Hernández, Suárez Falcón & Luciano, 2016). The basic techniques of ACT also don't necessarily need to be in a clinical setting either, making it more accessible and providing the implication that it could be used in educational or workplace settings as well as psychoeducation (Burckhardt, Manicavasagar, Batterham, Hadzi-Pavlovic & Shand, 2017; Cartwright & Hooper, 2017). REBT, CBT, MBCT, mindfulness and meditation are also effective ways to improve psychological flexibility and emotional health (Ellis & Joffe Ellis, 2011; Fledderus, Bohlmeijer, Smit & Westerhof, 2010; George & de Guzman, 2015). Also, increasing physical activity and getting outside into nature are also very beneficial to emotional well-being, while also improving your physical health.
See also
[edit | edit source]- Acceptance and commitment therapy (Wikipedia)
- Emotion perception (Book chapter, 2017)
- Flexibility (Wikipedia)
- Mental toughness (Book chapter, 2017)
- Psychological resilience development in children (Book chapter, 2017)
- Rational emotive behavior therapy (Book chapter, 2017)
References
[edit | edit source]Burckhardt, R., Manicavasagar, V., Batterham, P., Hadzi-Pavlovic, D., & Shand, F. (2017). Acceptance and commitment therapy universal prevention program for adolescents: a feasibility study. Child And Adolescent Psychiatry And Mental Health, 11, 2-10. https://doi:10.1186/s13034-017-0164-5
Cartwright, J., & Hooper, N. (2017). Evaluating a transdiagnostic acceptance and commitment therapy psychoeducation intervention. The Cognitive Behaviour Therapist, 10, 1-6. https://doi:10.1017/s1754470x17000125
Deak, A. (2011). Brain and emotion: Cognitive neuroscience of emotions. Review of Psychology, 18, 71-80. https://doi.org/orcid.org/0000-0001-6862-4993
Ellis, A., & Joffe Ellis, D. (2011). Rational Emotive Behavior Therapy. Washington DC: American Psychological Association.
Fledderus, M., Bohlmeijer, E., Smit, F., & Westerhof, G. (2010). Mental Health Promotion as a New Goal in Public Mental Health Care: A Randomized Controlled Trial of an Intervention Enhancing Psychological Flexibility. American Journal Of Public Health, 100, 2372-2372. https://doi:10.2105/ajph.2010.196196
George, B., & de Guzman, R. (2015). Effectiveness of acceptance and commitment therapy based intervention program (ACTP) on perceived stress and emotion regulation among alcoholics in Kerala, India. Indian Journal Of Positive Psychology, 6, 10-18. https://doi:10.4172/2329-6488.1000205
Gilam, G., Hendler, T. (2015). Deconstructing anger in the human brain. Current Topics in Behavioural Neurosciences, 30, 257-273. https://doi.org/10.1007/7854_2015_408
Gutierrez, D., & Hagedorn, W. (2013). The Toxicity of Shame Applications for Acceptance and Commitment Therapy. Journal Of Mental Health Counseling, 35, 43-59. https://doi:10.17744/mehc.35.1.5n16p4x782601253
Hall, K., Simpson, A., O'Donnell, R., Sloan, E., Staiger, P., & Morton, J. et al. (2018). Emotional dysregulation as a target in the treatment of co-existing substance use and borderline personality disorders: A pilot study. Clinical Psychologist, 22, 112-125. https://doi:10.1111/cp.12162
Harvey, S., Bimler, D., Dickson, D., Pack, J., Sievwright, O., Baken, D., Henricksen, A. (n.d.). Acceptance and Commitment Therapy Group Treatment with the Military: A Preliminary Study. Journal of Military and Veterans' Health, 26, pp.6-15.
Hayes, S. C, Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and Commitment Therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44, 1-25. https://doi:10.1016/j.brat.2005.06.006
Köhle, N., Drossaert, C., Jaran, J., Schreurs, K., Verdonck-de Leeuw, I., & Bohlmeijer, E. (2017). User-experiences with a web-based self-help intervention for partners of cancer patients based on acceptance and commitment therapy and self-compassion: a qualitative study. BMC Public Health, 17, 1-16. https://doi:10.1186/s12889-017-4121-2
Landstra, J., Ciarrochi, J., Deane, F., & Hillman, R. (2013). Identifying and describing feelings and psychological flexibility predict mental health in men with HIV. British Journal Of Health Psychology, 18, 844-857. https://doi:10.1111/bjhp.12026
Masuda, A., Price, M., Anderson, P., Schmertz, S., & Calamaras, M. (2009). The Role of Psychological Flexibility in Mental Health Stigma and Psychological Distress for the Stigmatizer. Journal Of Social And Clinical Psychology, 28, 1244-1262. https://doi:10.1521/jscp.2009.28.10.1244
Meyer, E., Frankfurt, S., Kimbrel, N., DeBeer, B., Gulliver, S., & Morrisette, S. (2018). The influence of mindfulness, self-compassion, psychological flexibility, and posttraumatic stress disorder on disability and quality of life over time in war veterans. Journal Of Clinical Psychology, 74, 1272-1280. https://doi:10.1002/jclp.22596
Montgomery, K., Kim, J., & Franklin, C. (2011). Acceptance and Commitment Therapy for Psychological and Physiological Illnesses: A Systematic Review for Social Workers. Health & Social Work, 36, 169-181. https://doi:10.1093/hsw/36.3.169
Nes, A., van Dulmen, S., Wicksell, R., Fors, E., & Eide, H. (2017). Analyzing Change Processes Resulting from a Smartphone Maintenance Intervention Based on Acceptance and Commitment Therapy for Women with Chronic Widespread Pain. International Journal Of Behavioral Medicine, 24, 215-229. https://doi:10.1007/s12529-016-9590-7
Pariyagath, V., Gowin, J., and Stein, E., (2015)., Resting state functional connectivity analysis for addiction medicine: From individual loci to complex networks. Progress in brain research, 224, http://dx.doi.org/ 10.1016/bs.pbr.2015.07.015
Pasanen, T., Tyrväinen, L., & Korpela, K. (2014). The Relationship between Perceived Health and Physical Activity Indoors, Outdoors in Built Environments, and Outdoors in Nature. Applied Psychology: Health And Well-Being, 6, 324-346. https://doi:10.1111/aphw.12031
Rait, S., Monsen, J. J., & Squires, G. (2010). Cognitive behaviour therapies and their implications for applied educational psychology practice. Educational Psychology in Practice, 26, 105-122. http://dx.doi:10.1080/02667361003768443
Reid, A., Garner, L., Van Kirk, N., Gironda, C., Krompinger, J., & Brennan, B. et al. (2017). How willing are you? Willingness as a predictor of change during treatment of adults with obsessive-compulsive disorder. Depression And Anxiety, 34, 1057-1064. https://doi:10.1002/da.22672
Robins, T., Roberts, R., & Sarris, A. (2015). Burnout and Engagement in Health Profession Students: The Relationships Between Study Demands, Study Resources and Personal Resources. Australasian Journal Of Organisational Psychology, 8, 1-13. https://doi:10.1017/orp.2014.7
Ruiz, F., Riaño Hernández, D., Suárez Falcón, J., & Luciano, C. (2016). Effect of a One-Session ACT Protocol in Disrupting Repetitive Negative Thinking: A Randomized Multiple-Baseline Design. International Journal Of Psychology And Psychological Therapy, 16, 213-233.
Sahebari, M., Asghari Ebrahimabad, M., Shoraketokanlo, A., Aghamohammadian Sharbaf, H., & Khodashahi, M. (2019). Efficacy of Acceptance and Commitment Therapy in Reducing Disappointment, Psychological Distress, and Psychasthenia among Systemic lupus Erythematosus (SLE) Patients. Iranian Journal Of Psychiatry, 14, 130-136. https://doi:10.18502/ijps.v14i2.992
Sairanen, E., Tolvanen, A., Karhunen, L., Kolehmainen, M., Järvelä-Reijonen, E., & Lindroos, S. et al. (2017). Psychological flexibility mediates change in intuitive eating regulation in acceptance and commitment therapy interventions. Public Health Nutrition, 20, 1681-1691. https://doi: 10.1017/s1368980017000441
Sandoz, E., Moyer, D., & Armelie, A. (2015). Psychological Flexibility as a Framework for Understanding and Improving Family Reintegration Following Military Deployment. Journal Of Marital And Family Therapy, 41, 495-507. https://doi:10.1111/jmft.12086
Spidel, A., Lecomte, T., Kealy, D., & Daigneault, I. (2017). Acceptance and commitment therapy for psychosis and trauma: Improvement in psychiatric symptoms, emotion regulation, and treatment compliance following a brief group intervention. Psychology And Psychotherapy: Theory, Research And Practice, 91, 248-261. https://doi:10.1111/papt.12159
Whittingham, K., Sanders, M., McKinlay, L., & Boyd, R. (2013). Stepping Stones Triple P and Acceptance and Commitment Therapy for Parents of Children with Cerebral Palsy: Trial Protocol. Brain Impairment, 14, 270-280. https://doi:10.1017/brimp.2013.19
External links
[edit | edit source]- Acceptance & Commitment Therapy Workshops (ACT Mindfully)
- DOI Display Guidelines Update (March 2017) (APA Style Blog)
- Get Out of Your Mind (Psychology Today)
- Headings (Grant State Valley University)
- The Happiness Trap (thehappinesstrap.com)
- The importance of structure (skillsyouneed.com)
- Psychological flexibility (Youtube)

