Motivation and emotion/Book/2016/Mental illness and treatment motivation
What role does treatment motivation play in managing mental illness?
Overview
[edit | edit source]This chapter considers how we define mental illness, and the impact it can have in terms of a person’s motivation and functioning. What are the lived experiences of mental Illness, and to what extent does the role of treatment motivation play in the management of mental illness? To a large degree this chapter aims to investigate the devastating effects of severe mental illness, and can motivation for treatment can be the whole solution. Notions of hope and recovery are vital. Two theories of motivation have been applied to the concept of treatment motivation and illness management. Finally the inclusion of artworks depicting the experience of mental illness have been included in this chapter. The reason for this is twofold, the first aims attempt to have a visual experience of the perceptual effects of mental illness as expressed by these artists. The second is to share in the wonder that such creative triumphs can be born out of such great difficulty.

Mental Illness
[edit | edit source]
Mental illness can be defined as a health condition that effects how a person thinks, feels or behaves. It can interfere with normal functioning and cause distress. The experience of mental illness can be varied and each mental health problem or illness can have different symptoms, and disrupt an individual’s life in different ways. The experience of a mental illness cause changes in a persons emotions, thoughts and behaviors, and may impair functioning and/or change the way a person thinks about themselves (National Survey of Health and Wellbeing,2009).
There are several different types of mental illness, these can include:
Table 1. Different Types of Mental Illness
| Mood Disorders | Effects mood/emotions. Depression and Bi-polar are two types of mood disorders |
| Anxiety Disorders | Anxiety and fear that cause avoidance of situations and events most people consider normal. Panic disorder and Post traumatic stress are anxiety disorders |
| Psychotic Disorders | Disruption in your ability to perceive what is real and what isn't (termed psychosis). Schizophrenia is the most commonly known psychotic disorder. May cause delusions, hallucinations, hearing voices and can effect speech, thought process and motivation |
| Eating Disorders | Distress and distorted thinking surrounding body image, resulting in significant changes in eating behaviour and weight loss. Can cause serious problems with malnutrition and strain on internal organs. Anorexia and Bulimia nervous are examples of eating disorders |
| Personality Disorders | Can influence the way a person thinks feels and acts and interrelates with others. May increase impulsive. Borderline personality disorder is an example of a personality disorder |
| Substance Use Disorders | A dependence on a substance such as alcohol, tobacco, and other drugs. (frequently called addiction.) |
| Dementia | Degeneration of brain cells, resulting in memory loss, altered judgement and reasoning and changes in mood, communication and behaviours (greater than seen in normal ageing). Alzheimer disease is the most well know form of dementia. |
| Attention Deficit /hyperactivity disorder (ADHD) | Most often found in children and youth, though can be diagnosed in adulthood. Interferes with focus of attention and can also include hyperactivity.
- Canadian Mental Health Association, (BC Division, 2016). |
|
The (DSM-5) states that to meet the criteria for a diagnosis of a mental health disorder, the set of symptoms or behaviors must cause clinically significant impairment or distress (American Psychiatric Association, 2013) |
Definition
[edit | edit source]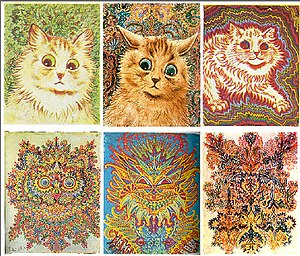
Treatment motivation is a construct now commonly held to be an essential and fundamental component to psychological treatment. Treatment motivation is willingness to engage, participate and adhere to psychological treatment (Dreischner, Lammer, & Staak, 2004). To achieve positive therapeutic outcomes, Krause (1966) argues that clients undertaking psychotherapy, counselling or receiving casework, must not be passive recipients of treatment but need to actively engage in treatment. This patient motivation:
"Is the vital factor in the outcome of the treatment." (Krause, 1996)
According to Lambert, Hurley, Tomlinson, and Stevens (2013), treatment motivation significantly influences how willingly an individual seeks out services, if they remain in treatment services or programs and enhances treatment outcomes. These authors argue that motivation for treatment is a critical element of mental health treatment, and is so integral to treatment outcomes that it needs to be evaluated as part of the treatment process. Earlier research from Ryan, Plant, and O’Malley (1995) attributes lack of treatment motivation as being the main basis for client drop out, non-compliance, and poor treatment outcomes.
For Di Clemente, Schlundt & Gemell, (2004) health motivation can be thought of in two conceptual domains, motivation to change, and motivation for treatment. Di Clemente explains that motivation to change is the recognition of distressing or challenging behaviors and the intent to make a change surrounding these. Whereas motivation to treatment influences how willingly an individual will seek, adhere and be compliant with treatment.
Dreischner, Lammer, and Staak (2004) argue that the concept of treatment motivation as “being highly relevant” they also argue that the construct of treatment motivation is ambiguous and there are problem in terms of conceptual confusion, ambiguous measures and contradictory research out comes.
For an exhaustive examination of the construct of treatment motivation: http://www.sciencedirect.com.ezproxy.canberra.edu.au/science/article/pii/S0272735803001107
Severe mental illness
[edit | edit source]
Severe mental illness such a schizophrenia, schizoaffective disorder bipolar disorder can have a devastating impact of people lives. For many the course of a severe mental illness is chronic and unrelenting (Mancini, 2008). Severe mental illness erodes a sense of self, impacts on relationship, and creates enormous difficulties in in work and gainful employment (Nordsy et al., 2002). Individuals affected by severe mental illness are frequently faced with living in poverty or become homeless, face stigmatization and socially isolated. For some, the destructive impacts of severe mental illness combined with messages of long term prognosis, become grounded in despair and lose hope for recovery (Nordsy et al., 2002).

Barrowclough, et al (2001) states that severe mental illness can impact on general health with poor diet, high rates of substance abuse and heavy smoking. Difficulties arise with managing self-care and basic hygiene. Severe mental illness affects individual global and social functioning, for some this mean independent living is not possible. Further to this, Nordsy et al (2002) argue that due to severe mental illness some individual become highly reliant on services, and may lose capacity for decision making. For some this can eventuate in involuntary admissions to psychiatric hospital or court ordered mental health treatment. For other where capacity is an issue this might include the appointment of guardians and financial trustees (Mancini, 2008).

Suicide
[edit | edit source]Of great concern is the high rates of suicide among those suffering severe mental illness,(Nordsy, et al. 2002). These authors state that building hope is essential to recovery. Without hope and a self-belief that one has the ability to make positive change, then a transition from chronic disability to functional recovery is very unlikely,(Mancini,2008). For Nordsy et al, (2002), hope for change is the wellspring of motivation, and motivation is the antecedent to action.
Path to recovery
[edit | edit source]The Role of History
[edit | edit source]Historically in Australia, mental health and mental illness were conceptualised in a very different way compared to today, adding to sense of stigma, sense of hopelessness and limited motivation to seek treatment.
It was assumed that people with mental illness:
- had no capacity to look after themselves
- should be separated from the rest of society
- were people considered ‘dangerous’
- should live in gaol or asylums
- some were considered ‘insane’ and seen to be responsible for their illness due to moral weakness and personal deficiency.
Human rights movement
[edit | edit source]Mental illness was out of sight, and mostly out of mind, however change slowly occured:
Table 1.
History and mental health related action
| Year | Action |
|---|---|
| 1838 | first large institution opened |
| 1859 | those with mental health problems were put in gaols alongside criminal offenders |
| 1869 | Lunacy Act was passed and the establishment of reception houses |
| 1884 | Insanity Act was passed |
| 1918 | first mental health ward opened in a general hospital, Brisbane |
| 1938 | Mental Hygiene Act |
| 1940s | Queensland based advocacy group formed, ' Relatives of the Mentally Ill Association' for patients with mental health issues |
| 1950s | new ideas emerged regarding psychiatric care which shifted from closed institutions and custodial care, to supporting patients to live in the community |
| 1960s/70s | a civil rights movement raised awareness of the rights of minority groups, including people with mental illness |
| 1961 | Mental Health Association was formed |
| 1974 | Mental Health Act |
| 1977 | Queensland Department of Health established office for advocacy on individual rights including the right to be consulted about treatment, the right to be protected from abuse, and the right to be free from unnecessary controls |
| 1992 | National Mental Health Strategy was approved comprising of the National Mental Health Policy, the First National Mental Health Plan, the Mental Health Statement of Rights and Responsibilities, a funding agreement between the Commonwealth and the states and territories |
| 1993 | Report of the National Inquiry into the Human Rights of People With Mental Illness |
| 2000 | Revised Mental Health Act |
| 2003 - 2008 | National Mental Health Plan |
| 2009 | Fourth National Mental Health Plan established |
| 2012 | Establishment of Mental Health Commission and Consumer Advisory Group. (The road to recovery - a history of mental health services in Queensland 1859-2009)
|
Consumer voices force change
[edit | edit source]The human rights movement evolved and the voices of patients themselves emerged as a force for change:
- balance of power shifted to place mental health service users on an equal footing with professionals
- it was recognised that mental health consumers have their own expertise in their knowledge of mental illness
- health policy began to support the active participation of consumers, families and carers in all aspects of policy, planning and services.
(The road to recovery - a history of mental health services in Queensland 1859-2009)
Recovery an alternative to the medical model
[edit | edit source]With the consumer movement, Recovery approaches were developed as an alternative to the medical model that had an emphasis on pathology, deficits and dependency. Central to all recovery paradigms are hope, self-determination, self-management, empowerment and advocacy. Also key is a person's right to full inclusion and to a meaningful life of their own choosing, free of stigma and discrimination.
Some characteristics of recovery commonly cited are that it is:
- a unique and personal journey
- a normal human process
- an ongoing experience and not the same as an end point or cure
- a journey rarely taken alone
- nonlinear—frequently interspersed with both achievement and setbacks.
Recovery and the mental health system
[edit | edit source]The principles of recovery-oriented mental health practice was introduced to ensure that mental health services are delivered in a way that supports the recovery of mental health consumers and meets all 10 requirements of the national standards.
The Australian Department of Health outlines in further detail, the principles of recovery oriented mental health practice which apply to the entire mental health service system. They include consideration to the following themes:
- Uniqueness of the individual
- Real choices
- Attitudes and rights
- Dignity and respect
- Partnership and communication
- Evaluating recovery

| "From the perspective of the individual with mental illness, recovery means gaining and retaining hope, understanding of one's abilities and disabilities, engagement in an active life, personal autonomy, social identity, meaning and purpose in life, and a positive sense of self.
It is important to remember that recovery is not synonymous with cure. Recovery refers to both internal conditions experienced by persons who describe themselves as being in recovery – hope, healing, empowerment and connection – and external conditions that facilitate recovery – implementation of human rights, a positive culture of healing, and recovery-oriented services".(Jacobson and Greenley, 2001 p.482) |
Motivational Paradox
[edit | edit source]
Is motivation always enough?
[edit | edit source]|
Julia arrives to the door of her work early one morning to find her friend David she hasn’t seen for some time. David is dressed in a suit, with briefcase in hand. Something is off. David lives, and works in another city. David tells Julia he has hitched a lift overnight with a truck driver because he is under surveillance from the government, and needs to get out of the state. Can he please stay with her because she lives in Victoria? Julia tells David he is very welcome to stay with her. Once Julia can leave work, David returns in beach attire and has discarded his suit and briefcase and is desperate to be driven out of NSW. At first, Julia tries to carry on as though this is a normal social visit, but as the evening unfolds is David becoming more frightened, is having auditory hallucinations and is pacing and shouting into the night air at unseen people. Any written material viewed by David contains hidden and threatening messages. By early morning David has rearranged the furniture to make safety barriers and is clinging for dear life to Julia’s hand. At no time can Julia discuss David mental state because it only serves to increase David's paranoia. Julia drives David 300 kilometers to Melbourne to see his Psychiatrist and David is admitted to a mental health unit. This was not the first, or last time David had a Schizophrenic relapse but it was certainly one of the most severe.
|
Motivational Paradox
[edit | edit source]The motivation paradox refers to a subset of people suffering with severe mental illness, who the more unwell they become,the less they seek, but more they need treatment.
Mulder, Jochems and Kortrijk (2016) argue that lack of motivation for psychiatric treatment can be associated with severe mental illness (SMI). People with SMI are often the most in need of treatment, and there is an inverse relationship between increased psychosocial problems and treatment motivation. The enduring effects of psychosis and chronic psychiatric conditions are found to negatively impact on the ability to manage mental illness. Mancini (2008), who has done considerable work in the area of recovery, states that SMI erodes a person's capacity to initiate treatment seeking behaviors, and their ability to voice preferences.
For Mulder, Jochems and Kortrijk (2016), the motivational paradox results in low motivation to seek treatment, noncompliance with mental health plans, resistance to treatment due to previous treatment experiences, or the belief that treatment be may be of no benefit.
Other barriers to treatment motivation may be disabilities or intrinsic impairment such as lack of insight. Forgetting to attend appointments and reluctance due to negative stereotype surrounding mental illness are also a contributing factors.
This research and others indicates that individuals with persistent and acute SMI left untreated have much poorer health outcomes. Mulder, Jochems and Kortrijk (2016) pose this as an argument for the continuation of assertive outreach programs. They also argue that this evidence provides support on an ethical basis for paternalistic practices such court mandates to treatment facilities, or medication.
Self-Determination Theory and Treatment Motivation
[edit | edit source]To understand Self-Determination Theory in terms of treatment motivation, it is helpful to think of motivation along a scale of self-determination (Jochems et al., 2014). At one end of this continuum is the highest level motivation which is intrinsic, followed by integrated, identified, and introjected, to the other end which is external or amotivation (Ryan & Deci, 2000).
Intrinsic
[edit | edit source]A person with high intrinsic motivation for treatment willingly seeks out mental health treatment, and is motivated by the inherent value or pure satisfaction of the treatment. While this high level of motivation to engage is deemed as optimal for long term positive results. Jochems et al. (2014) state that this motivation is unusual, as more often people are seeking treatment solely for symptom relief.
Integrated
[edit | edit source]Integrated motivation for treatment can be seen in an individual who not only values treatment for symptom relief but has integrated the long term value of sustained well-being as part of their self-concept (Jochems et al., 2014). This is a patient who continues to seek treatment as an outpatient after hospitalization and wants to continue treatment as a maintenance. Or perhaps, is the individual who on completion of a treatment program, enrolls in a support group or new treatment program with the motivation to sustain longevity of mental health in mind (Ryan & Deci, 2008).
Identified
[edit | edit source]Identified motivation for treatment is when a person sees treatment and medication as a means to an end, or to avoid relapse. Identified motivation differs from integrated motivation because it is more functionally based than an integrated part of self-identity (Jochems et at., 2014).
Introjected
[edit | edit source]Lower on the self-determination continuum is introjected motivation for treatment, which may be driven by feelings of shame and anxiety. Adherence to treatment is motivated by feeling of remorse for past behaviours or to avoid feelings of guilt for treatment nonattendance (Jochems et al., 2016).
External
[edit | edit source]External motivation to treatment is when a person is coerced into treatment by a concerned parent, a partner on the verge of ending the relationship, or when an individual is so unwell that they have been mandated to treatment by the judicial system. According to Jochems, et al. (2014) this is the most problematic approach to long term mental health outcomes as the person may only seek treatment or adhere to medication if this external motivation is applied (Jochems et al., 2014).
Amotivation
[edit | edit source]Self Determination theory sees amotivation to treatment as when a person doesn’t have a clear picture of the value of treatment engagement. Who has little hope of treatment success, or an expectation of treatment failure and is most likely to drop out or disengage with treatment (Jochems et al., 2014). From this we can understand the more self-determined an individual is to engage with treatment the more likely they are to receive beneficial outcomes and fulfill their personal goals, whereas, the more reliant a person is on external motivators the less likelihood of successful long term management (Ryan & Deci, 2008).

Autonomy Competence and Relatedness
[edit | edit source]According to Jochems (2016), the psychological needs of autonomy, competence, and relatedness are psychological underpinnings to the motivations types in the self-determination theory framework. People who are high on self-determination because their psychological needs of autonomy, competence, and relatedness have been met, are more likely to be intrinsically motivated (Matusitz & Martin, 2013).
Autonomy
[edit | edit source]To use the mental health disorder of Anorexia nervosa as an example of this concept; an individual who has a grounded sense of autonomy, may in relation to media and societal pressures to be thin, have good control and choose healthy eating behaviors and exercise to lose weight. Whereas, a person who has poor sense of autonomy and low self-determination may engage in disordered and uncontrolled eating behaviors resulting in an eating disorder such as anorexia and bulimia nervosa (Matusitz & Martin, 2013).
Competence
[edit | edit source]Competence can be defined as effectively managing the demands of one's environmental and relational contexts. To meet the need for competence, an individual will perceive they are able confidently manage and achieve goals. For an individual who is struggling with feeling capable of effectively meeting their goals to become to lose weight this may then transpire that disordered eating become the most manageable option.
Relatedness
[edit | edit source]Relatedness refers to the accessibility of meaningful and trustworthy relationships. In the case of an individual suffering with Anorexia who may try to keep the illness secret and not trust in others and therefore not seek help and treatment to manage this mental illness. For Ryan and Deci (2008), relatedness is the need to feel valued and connected to others. Thus a treatment program or therapeutic environment that can build upon an individual’s ability to harness the dynamics of relatedness, autonomy, and competence, to support a more intrinsically motivated and integrated motivation for treatment success, and the achievement of personal goals.(Matusitz & Martin, 2013).
Trans-theoretical model (stages of change)
[edit | edit source]
The Trans-theoretical-stage of change model (TTM) was developed by James Prochaska and Carlo Di Clemente in the 1980’s, to explain individual differences in motivation and readiness for change surrounding substance use and misuse. The TTM model operates under the assumption that people differ in their readiness to change, where they are in the cycle of change, and fluctuate in terms of how permanent they want the changes to be (Vancampfort, Stubbs, Venigalla & Probst, 2015).
In this behavior change model the different stages are pre-contemplation, contemplation, preparation, action and maintenance. An individual’s movement through these stage are seen to be influenced by three factors (process of change, decisional balance, and temptation/ self-efficacy). The TTM model operates in the therapeutic context under to identifying which position a person is in ,and aims to match appropriate interventions (Kortrijk et al., 2013).
While there has been much attention to the TTM model in terms of motivation to change with substance abuse, this model has also been found to be applicable to individuals with SMI, particularly because there are such high rates of co-morbidity between substance abuse and SMI (Drapalski, Bennet &Bellack, 2011).
Di Clemente, Nicker & Black, (2006) have argued that as many as 50% of people with acute and persistent SMI such as schizophrenia and bipolar disorder meet the criteria for substance use disorder (SUD) in their lifetime. Substance abuse for those struggling with SMI creates a harmful and complicating factor as it exacerbates symptoms, creates difficulties with treatment engagement. Other adverse consequences are found to be noncompliance with medication, hospitalization, and diminished motivation. Individuals with a dual diagnosis of SUD and SMI are less likely to achieve positive outcome and more likely to relapse than those with SMI alone (Di Clemente, Nidecker& Bellack, 2006).
To understand the motivational and behavior change process, it can be thought of as a progression through the various stages or states. The give stages are:

- Pre- contemplation (no inclination to modify behavior)
- Contemplation, (reflection problem but not yet committed to take action)
- Preparation (planning to implement action in near future)
- Action (modification of behavior)
- Maintenance (relapse avoidance and consolidation of achievements).
Prochaska and Di Clemente (1992) suggest that this can be can conceived of as a spiral model of motivation, whereby individuals progress up and down the spiral, through states of changes before exiting. Some people may repeat this cycle and relapse many times, or remain in the maintenance phase, whereas other may reach exit and terminate the process (Dray & Wade 2012).
The Trans-theoretical model has been widely been applied to treatment programs for substance abuse, treatment of dual diagnosis of SMI and SUD, (Dray & Wade, 2012). Earlier research from Prochaska and Velicer (1997) on the applicability of the TTM model as a change intervention, found positive outcomes in individualized computer generated counselling session. The potential benefit of which, they argue, is that these interventions can be made widely available to the general population.
Dray & Wade’s (2012) TTM research indicated positive results for the treatment of eating disorders. They argue these findings are important because of the difficulties in treating eating disorder due to the incongruence between self-image, needs and recovery. Other impediments are ambivalence to treatment, denial of the problem, and distress caused by weight gain. Given this resistance, and the protracted and chronic course an eating disorder can run leading to detrimental social, and health outcomes including high rates of hospitalization and mortality. Any treatment found to ameliorate these effects is valuable indeed. Dray and Wade (2012) found that the stages of change model was relevant in increasing confidence to change, improved treatment adherence and relapse prevention.
TTMs have been applied to assist with improving motivation for general health behaviors as well as to those suffering mental illness. Farholm and Sorensen (2016) argue that those experiencing SMI, such as schizophrenia, bipolar disorder and major depression are at increased risk to health, as these disorders are commonly associated with high levels of smoking, excessive drinking behaviors in combination with poor diet and physical inactivity. Vancampfort, Stubbs, Venigalla, & Probst, (2015) also argue that individuals with SMI, have much lower rates of life expectancy due to cardiovascular disease.
Moreover, while they state that psychical activity enhances mental as well as psychical health and improves the quality of life for individual with SMI. These authors go to say that only a small percentage of people with SMI engage in exercise or psychical activity at public health recommendations. This has been attributed to psychiatric symptoms, disinterest, and low motivation. SMI also impact on a sense of competency to transfer physical activity goals into action. Vancampfort, Stubbs, Venigalla, & Probst, (2015) found that interventions that facilitated changes in behavior and increased intrinsic motivation where played an important in increasing adherence to psychical activity and improving health outcomes.
Conclusion
[edit | edit source]Treatment motivation has a substantial role in the management of mental illness. Motivation for treatment supports treatment and medication adherence, and facilitates treatment engagement, a crucial aspect to treatment success. For those individuals dealing with severe mental illness, issues of hope and recovery are pertinent, however some severe mental illness can have such a great impact that it creates a motivation paradox. Whereby, the most in need of treatment, have the greater difficulty to overcome. Self- determination theory explains a continuum from intrinsic to extrinsic motivation. These motivation types, in combination with the psychological needs of autonomy, competence, and relatedness offer insight into possible treatment approaches. The trans- theoretical stages of change model help us understand how individuals cycle through the stages of change, to hopefully to exit to lasting good health.
See also
[edit | edit source]- Anorexia nervosa and extrinsic motivation (Book chapter, 2016)
- Artistic creation motivation (Book chapter, 2016)
- Mental health help-seeking motivation (Book chapter, 2016)
- Overcoming social stigmas (Book chapter, 2016)
References
[edit | edit source]Di Clemente, C. C., Nidecker, M., & Bellack, A. S. (2008). Motivation and the stages of change among individuals with severe mental illness and substance abuse disorders. Journal of Substance Abuse Treatment, 34(1), 25-35.http://dx.doi/org/10.1016/j.jsat.2006.12.034
Di Clemente, C., Schlundt, D. & Gemmell, L. (2004). Readiness and stages of change in addiction treatment. American Journal on Addictions, 13, (2),103-119. http://dx.doi.org/10.1016/j.jsat.2006.12.034
Drapalski, A., Bennett, M., & Bellack, A. (2011). Gender differences in substance use, consequences, motivation to change, and treatment seeking in people with serious mental illness. Substance Use & Misuse, 46(6), 808-818. doi: 10.3109/10826084.2010.538460
Dray, J., & Wade, T. D. (2012). Is the transtheoretical model and motivational interviewing approach applicable to the treatment of eating disorders? A review. Clinical psychology review, 32(6), 558-565. http://Doi:.org/10.1016/j.cpr.2012.06.005
Drieschner, K. H., Lammers, S. M., & van der Staak, C. P. (2004). Treatment motivation: An attempt for clarification of an ambiguous concept. Clinical Psychology Review, 23(8), 1115-1137. Retrieved from http://dx.org/10.1016/j.cpr.2003.09.003
Jochems, E. C., Mulder, C. L., Duivenvoorden, H. J., van der Feltz-Cornelis, C. M., & van Dam, A. (2014). Measures of Motivation for Psychiatric Treatment Based on Self-Determination Theory Psychometric Properties in Dutch Psychiatric Outpatients. Assessment, 21(4), 494-510. doi: 10.1177/1073191113517928
Krause, M. S. (1966). A cognitive theory of motivation for treatment. The Journal of General Psychiatry, 75, 9–19. Retrieved from http://www.tandfonline.com/doi/abs/10.1080/00221309.1966.9710345
Kortrijk, H. E., Mulder, C. L., van Vliet, D., van Leeuwen, C., Jochems, E., & Staring, A. B. P. (2013). Changes in motivation for treatment in precontemplating dually diagnosed patients receiving assertive community treatment. Community mental health journal, 49(6), 733-741 doi: 10.1007/s10597-012-9582-2
Lambert, M., Hurley. Tomlinson. & Stevens, A. (2013). Measurement properties of the motivation for youth treatment scale with a residential group home population. Child Youth Care Forum, 42, 555-570. doi:10.1007/s10566-013-9217-y
Mancini, A. (2008). Self-determination theory: a framework for the recovery paradigm. Advances in Psychiatric Treatment, 14, (14), 358-365 doi:10.1192/apt.bp.107.004036
Matusitz, J., & Martin, J. (2013). The application of Self-determination theory to eating disorders. Journal of Creativity in Mental Health, 8(4), 499-517. doi: 10.1080/15401383.2013.850392
Mulder,C., Jochems,E. & Kortrijk,H. (2014). The motivation paradox: higher psychosocial problems levels in severely mentally ill patients are associated with less motivation for treatment. Soc Psychiatr Epidemiol, 49, 541-548, doi:10.1007/s00127-013-0779-7
Nordsy, D., Torrey. Mueser,K., Mead, S., O’Keefe, C., & Fox,L. (2012). Recovery from severe mental illness: an intrapersonal and functional outcome definition. International Review of Psychiatry, 14, (4), 318-326. doi: 10.1080/0954026021000016969
Ryan, R., & Deci, E. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55, 68–78. doi:10.1037/0003-066X.55.1.68
Ryan, R. M., & Deci, E. L. (2008). A self-determination theory approach to psychotherapy: The motivational basis for effective change. Canadian Psychology, 49, 186-193. doi:10.1037/a0012753
Ryan, R. M., Plant, R. W., & O’Malley, S. (1995). Initial motivations for alcohol treatment: Relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors, 20, 279–297. doi: 10.1016/0306-4603(94)00072-7
Slade ,T.,Johnson ,A Teeson, M. ,Whiteford,H., Burgess,P.,Pirkus,J.&Saw,S.(2009) The Mental Health of Australians 2. Report on the 2007 National Survey of Mental Health and Wellbeing, Department of Health and Aging, Canberra.
- Resources needing improved grammar
- Resources needing clarification
- Resources needing facts checked
- Resources needing clarification by what
- Motivation and emotion/Book/2016
- Motivation and emotion/Book/Mental health
- Motivation and emotion/Book/Self-determination theory
- Motivation and emotion/Book/Treatment motivation
