Motivation and emotion/Book/2015/Climate change and mental health
What is the effect of climate change on mental health?
Overview
[edit | edit source]
Climate change
[edit | edit source]
Climate change refers to changes in meteorological parameters. Over the last 150 years, the earth's climate patterns have altered by excess carbon dioxide (CO2) trapped in the atmosphere (Schlesinger, 2011). Carbon dioxide is a naturally occurring gas necessary for survival and is emitted through living things, too much of this chemical compound, however, is pollution. Carbon pollution, also known as global warming, increases through human activity: clearing of land (deforestation); transportation; industrial processes and the burning of fossil fuels (coal, oil, gasoline) to make energy. Precipitation and temperature rises have great impact on the environment with the severity of natural disasters and sea levels increasing as a result of warming temperatures (Padhy, Sarkar, Panigrahi & Paul, 2015). As water temperatures change, ice caps melt, ocean acidity increases, coastal ecosystems are threatened and lower grounded areas face potential floods and danger of submergence. Through impacting the environment, climate change also threatens food supply, economical status and the physical and mental health of individuals within affected societies. Specific environmental conditions affect individuals in a range of ways.
A critical correlation exists between climate change and depression, as well as its related psychological challenges. Challenges of climate change have been observed to heighten incidences of mental and social disorders that include depression, post-traumatic tension, drug use, suicide and violent behavior. Marginalized communities are observably the worst hit, particularly those in developing nations, with children, the elderly, the poor and people with existing health disorders being the most vulnerable. Current health institutions in diverse nations are not sufficiently capable of handling mental challenges resulting from climate change.
Mental Health
[edit | edit source]|
"Mental health is defined as a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community" (World Health Organisation, 2011) |
An individual's mental health is measured by their total well-being (physical, mental and social). Mental health disorders affect developing countries by 35 per cent more than those in developed countries due to the accessibility of available health care. Other factors that may influence the development of mental health disorders include gender, age, socioeconomic status, demographic factors, biological factors, family environment, inequalities and diet (Rafique, 2013; Fernandes, 2013; Egger & Emde, 2011). Mental health is a primary aspect in achieving ideal well-being. Promoting mental health is vital whether through the workplace, education system or media (Riasat, 2013). Optimal mental health can influence an individuals relationships, concentration, behaviour and overall well-being. There are many available options in the treatment of mental health disorders:
- Antidepressants: tricyclic antidepressants, monoamine oxidase (MAO) inhibitors, elective serotonergic reuptake inhibitors (SSRIs), mixed reuptake inhibitors
- Psychological treatments: Cognitive behavioural therapy (CBT), Interpersonal psychology (IPT), behavioural activation, psychodynamic therapy
- Others: community support programs, hospital treatment
(Klerman, Weissman, Rounsaville & Chevron, 1984; Marks, Shaw & Parkin, 1998; Clarke, Rodhe, Lewinsohn, Hops & Seeley, 1999)
The fifth edition Diagnostic and Statistical Manual of Mental Health Disorders is the most recently updated manual published by the American Psychiatric Association (APA). This manual identifies hundreds of mental health issues through diagnostic criteria including neurodevelopmental disorders, psychotic disorders, trauma related disorders, substance related disorders and depressive disorders. Alterations have been made constantly to keep the manual updated with current research findings. The most recent update in 2013 saw the removal of the multi-axial system to implement a simpler form of categorisation (Tannock, 2013). |
Climate conditions effect on mental health
[edit | edit source]High Ambient Temperatures
[edit | edit source]Ambient temperature is the surrounding environment's heat level, with the earth's temperature increase, heat exposure is common. According to research, high temperatures have suggested being linked to aggressive behaviour, criminal activity, suicide rates, mental and behavioural disorders. Similarly, extreme heat or heat waves are associated with psychological distress, dementia, substance abuse, eating disorders and physical and mental exhaustion (Padhy et al., 2015; Berry, Bowen & Kjellstrom, 2010).
Individuals notice the impact heat has on their mental capacity regularly as their concentration and working capacity decreases during hotter seasons. A high core body temperature and dehydration are primarily responsible for these effects. It has been suggested that the intense rise or fall of temperature is what affects mental health rather than the temperature itself (Berry, Bowen & Kjellstrom, 2010). High temperatures can disrupt a person's thermoregulation (the body's ability to regulate it's core temperature despite the surrounding temperatures), especially those with mental illness, due to medication or illness factors. The body's thermoregulation is impaired by certain medication prescribed for mental illness (specifically those with dementia), increasing vulnerability during hot weather. Research recognised during periods of peaked temperature, individuals with mental illness seeking medical attention also increased. A suggestion for this increase may be temperatures ability to alter biological chemicals such as plasma tryptophan, serotonin, brain serotonin, and platelet serotonin. Furthermore, specific illnesses may affect an individual's cognitive ability, influencing their judgement on temperature and preventative measures (Wang, Lavigne, Ouellette-kuntz & Chen, 2014; Hansen, Bi, Nitschke, Ryan, Pisaniello & Tucker, 2008).
Natural Disasters
[edit | edit source]Natural disasters are naturally occurring processes which create severe, sudden environmental events: floods; bush fires; tsunamis; volcano eruptions and earthquakes each impact their surroundings in different ways. Extreme anxiety disorders (ie. post traumatic stress disorder), for example, have been linked to floods, bush fires, heat waves and cyclones. More specifically, floods are responsible for long term depression and anxiety, PTSD and increased depression. Individuals may react differently depending on the direct or indirect nature of specific climate events as well as it's frequency, intensity and duration (Berry, Bowen & Kjellstrom, 2010). After natural disaster has struck, medical assistance is a primary necessity although medical professionals have also identified the need for psychological responses. Individuals will react differently depending on their experience or exposure to the disaster. Victims may be affected directly or indirectly by disasters, creating specific clinical assessment and treatment (Galambos, 2005). Disaster psychiatry is a newly observed psychiatric discipline used to explore the mental health of individuals after they experience a disaster. As disasters have struck around the world, clinicians explored the severe connotations involved impacting mental health (Reifels, Naccarella, Blashki & Pirkis, 2014). Despite post traumatic stress disorder being less known in Japan until the mid to late 199's, symptoms of the illness was recognised in Asia as a result of the continents susceptibility to natural disasters. A study following an earthquake in Asia saw the 142 participants experiencing sleep disturbance, depression, hypersensitivity and irritability as a result. Short term anxiety and depressive disorders were also consistent in the study, revealing unemployment, financial costs, home reconstruction, physical fatigue and relocation being the primary sources (Kokai, Fujii, Shinfuku & Edwards, 2004).
Drought and Suicide
[edit | edit source]Drought is the shortage of water caused by extended periods of little rainfall and provides a negative impact for any affected environments. It has been suggested that climate change will increase the frequency and severity of drought (Edwards, Gray & Hunter, 2014; 2015). Farmers have an elevated risk of suicide and are particularly impacted by these prolonged periods because the dry environment and little precipitation affects the growth of crops (McFarlane & Van Hooff, 2013). The impact on crops may lead to financial issues and with insufficient access to mental health assistance being in rural areas, farmers are at a greater risk of developing depression due to the pressure of providing (Padhy et al., 2015). The exposure to chemicals such as pesticides in agricultural occupations has been linked to neurological changes which may also suggest farmers susceptibility to depressive symptoms (McFarlane & Van Hooff, 2013). It is also expected that farmers suffer mentally from drought due to personal loss: livestock and vegetation, for example. Furthermore, studies show farmers in drought prone areas have a 4 per cent higher risk for having mental health issues than farmers in other areas. Due to climate change, drought will continue to primarily affect farmers (Edwards, Gray & Hunter, 2014; 2015).
Predicted global climatic changes are said to exacerbate cases of drought. This poses severe mental related consequences because drought and depression have a critical correlation. The predicted climatic changes will cause flooding of some areas while drought will critically hit some areas. Recent cases of farmer suicides owing to drought have been observable, and mitigation measures ought to be implemented to prevent the widespread of this mental challenge (Pearce et al., 2015). Crop failures automatically lead farmers to economic hardships, and those who cannot endure the consequential challenges often resort taking their lives. Cases of violence have been reported, owing to the hot weather that results from drought. Furthermore, a greater number of individuals have engaged in drugs owing to the hot weather, and suicide cases resulting from drug use are rampant (Singh & Purohit, 2014).
Effect on Circumstance
[edit | edit source]Migration and Vocational Changes
[edit | edit source]Climate related disasters influence individuals to relocate their families from dangerous areas. As climate change intensifies the severity of natural disasters, lives are at risk and diseases spread as homes and communities are destroyed. The impositions created by climate change affect communities on a physical and emotional level. After disaster has struck an area, occupants may become distressed considering the future of those around them and decide relocation to a safer location is necessary (Berry, Bowen & Kjellstrom, 2010). Experiencing the uncertainty about the future and the implications of the disaster negatively impacts the mental health of victims. As families evacuate or migrate, stresses are created through the relocation, especially when victims had established a sense of community (predominantly Indigenous communities). Distress may be intensified when evacuation is time sensitive as families don't have the luxury of processing the circumstances or retrieving belongings (Felix, Afifi & Afifi, 2012).
Severe climatic changes are usually associated with community relocations, as people seek safer environments for settlement. These migrations often result in community disruptions and professional change, and this may have severe socioeconomic impacts on such affected communities. For example, the infamous Hurricane Katrina that struck New Orleans in 2005 posed significant economic, physical and mental challenges to the survivors. This event resulted in the displacement and obligatory resettlement of nearly half a million inhabitants of the city, with the re-settlements being both permanent and temporary (Pearce et al., 2015). The livelihoods of most of these individuals were lost during the settlements while other individuals experienced career change. This meant a reduction in their earnings, and hence resulting in mental disorders. A survey of some survivors indicated that virtually all the assessed individuals confirmed symptoms of post traumatic stress disorder. However, these symptoms are said to decrease over time, as the affected populace adjusted to the new environment and vocations (Thomas et al., 2014).
Rural and Urban Areas
[edit | edit source]Rural areas are spaces made up of undeveloped land with low population density. These regions are distanced from urbanisation making them ideal farming regions. Urban areas are developed sectors consistent of a heavy population density, commercial buildings, bridges and railways (e.g. towns or cities). Health care, although widely available, may be less accessible in remote areas compared to urban societies. Regions exposed to natural disasters benefit from support of the community, meaning smaller communities provide a more intimate recovery (Felix, Afifi & Afifi, 2012). The sudden impact of disasters create the need for communities to act quickly, urban areas with higher population density means effective assistance when necessary. Rural areas are limited by resources and rely on surrounding urban areas in cases of emergency (Galambos, 2005).
Farming communities and regions dependent on the growth of crops, especially in developing countries, may suffer from malnutrition and a lack of finances because of fluctuating precipitation levels. Studies examining the association between drought and mental health exposed regional and rural areas prone to drought to demonstrate a higher percentage of mental health issues (Edwards, Gray & Hunter, 2014;2015; OBrien, Berry, Coleman & Hanigan, 2014).
Socioeconomic Status: Developed versus Developing countries
[edit | edit source]An important aspect to consider is the socioeconomic status of those within affected societies. Those suffering a monetary disadvantage will rely upon developed countries for assistance (Berry, Bowen & Kjellstrom, 2010). The World Health Organisation (2010) estimating the majority (75%) of those suffering from mental health disorders living in developing countries didn't have sufficient access to the appropriate care. A recent survey indicates that adverse climatic change mental impacts are observable in both developed and developing nations. The mental impacts on the population are almost similar (Cunsolo et al., 2015). However, it is the response to these psychological impacts that differs among the developed and the developing nations (Weissbecker, 2011). The recent catastrophic climate occurrence that include the Pakistani floods, the China landslides, heat, drought and wildfires in Russia and the US heat wave left devastating effects on life and property. The resulting depression on the affected individuals was even more challenging, as people recalled their lost loved ones and property (Dogra et al., 2012). Experts reveal that survivors exposed to more severe and intense disastrous events were observed to have severe mental challenges than the ones exposed to milder events.
Causative climatic factors differ between developed and developing nations. For instance, in the developing nations such as in Africa, farmers were observed to experience mental disorders owing to diverse floods that affected their crops thus leading to losses. Losses of lives and property owing to such floods were also evident (Butler, 2014). A change in the rainfall patterns where there was little or no rain was also a stress-causing agent to such farmers. On the other hand, failed rains did not appear to stress individuals in developing nations, who were well prepared and had implemented sophisticated farming inputs and methods. Catastrophic events that included various hurricanes and heat waves were observed to be the key causes of concern to individuals in developed nations (Ghatge & Rasal, 2013).
As indicated, the response to the climatic changes differs significantly between the developed and developing nations. The developed nations, perceived to be more advanced economically and socially, observably implement improved preparation measures than their developing nations counterparts. Such nations have better disaster management and enough funding to relocate affected communities during severe climatic changes (Sharma, Atri & Branscum, 2013). The developing nations will mostly depend on foreign aid in the form of funding and expertise during the emergence of various catastrophic climate changes. This serves to heighten the mental disorders on the affected communities, and the mitigation measures for the consequential mental illness are usually below average (Kronlid, 2014). The inadequacy of health institutions and mental health workers often worsen the challenge of climatic mental disorders in developing nations.
Physical Health effects of climate related events
[edit | edit source]There is a definite link between mental and physical health. Due to physical illness, psychological distress may arise and vice versa. Due to environmental impacts, high temperatures, floods and drought have been associated with cardiovascular disorders, respiratory disorders, gastrointestinal disorders and renal problems (Padhy et al., 2015). A lack of food and the development of water and vector borne diseases will also arise due to exposure to high temperatures (Hofmeijer et al., 2013;2012). Exposure to acute weather conditions means individuals are vulnerable to the physical dangers of their surroundings (Berry, Bowen & Kjellstrom, 2010). The dangers of unpredictable weather events increase the rates of morbidity and mortality within societies (Cunsolo Willox et al., 2015;2014). Those who are younger, physically impaired or elderly are particularly vulnerable to dangerous weather conditions as they are less able to defend themselves from the elements without assistance from those more capable. The elderly, for example, are more susceptible to the affects of high temperature due to multi-organ dysfunction which can lead to death (Hansen et al., 2008). A study by Watkiss and Hunt (2012;2011) recognised a significant increase by year 2080 in premature deaths due to the increasing temperatures of climate change (from 20,000 to 160,000 deaths). Society must also be aware of the increasing particles and gases in the environment affecting our health (e.g. dust, allergens, water vapour). Specifically, wildfires and drought increase smoke, dust and pollen particles in the air which can affect peoples respiratory and cardiovascular systems (Tibbetts, 2015).
Maslow's Hierarchy of Needs
[edit | edit source]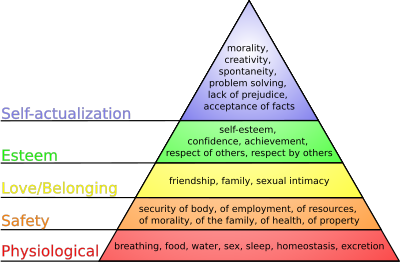
Abraham Maslow developed a five tier theory of needs: physiological; safety; belongingness; esteem and self-actualisation (see figure 2). In order for higher tiers to be fulfilled, lower tiers must first be achieved. Each need identifies different aspects of an individuals life and is satisfied depending on potency:
- Physiological: include necessities such as food, water, shelter, sexual needs and sleep
- Safety: includes security, stability, dependency and the absence of fear, anxiety and chaos
- Belonging: involves healthy relationships with friends, lovers and family members
- Esteem: is having respect of self, respect of others, achievement, adequacy, mastery and competence
- Self-actualisation: involves individuals using their abilities and talents appropriately
|
Similarly, the Need Satisfaction Inventory (Lester, 1990) measures the level of satisfaction of each concept through a survey comprised of fifty statements to be completed by the patient which is answered and measured on a five point scale of agreeableness (Deckers, 2010). |
Maslow proposed that everyone has the same needs although depending on circumstances in culture and the individual, fulfillment of needs may vary. Environmental events unquestionably challenge the fulfillment of needs by causing instability. Although some may never achieve self-actualisation, all human beings have a right to basic needs (Harper, Harper & Stills, 2003). Climate change may affect a person's ability to acquire such needs as clean drinking water and shelter as a result of drought. By taking away these necessities, safety is unable to be attained (Taormina & Gao, 2013). Generally, the impacts of climate change will directly impact physiological, safety and belonging needs while indirectly impacting the higher two tiers. Loss of friends or family, home destruction, insufficient water and sources of food and fear increased by lack of safety all contribute to the inability to achieve need satisfaction.
Conclusion
[edit | edit source]A vital association has been observed between climate change and mental challenges. Severe climatic changes have been linked to people’s symptoms of diverse stress disorders that include anxiety, depression and other related problems such as violence and drug use. Extreme cases of suicide are also evident, where farmers take their lives owing to failed crops. The regional communities are perceptibly the worst hit, particularly those in developing nations, with children, the elderly, the poor and people with other prevalent health challenges receiving the biggest blow. Socioeconomic features of a nation are critical in determining the extent of such effects, and the intervention measures. Relocation and career changes owing to climate changes pose diverse mental as well as economic hardships to the affected populace, and timely and effective mitigation measures ought to be implemented.
Test Yourself
[edit | edit source]
References
[edit | edit source]- Berry, H. L., Bowen, K., & Kjellstrom, T. (2010). Climate change and mental health: A causal pathways framework. International Journal of Public Health, 55(2), 123-132. doi:10.1007/s00038-009-0112-0
- Butler, C. D. (2014). Climate Change and Global Health. Canberra: CABI Publishers.
- Clarke, G. N., Rodhe, P., Lewinsohn, P. M., Hops, H., & Seeley, J. R. (1999). Cognitive-behavioral treatment of adolescent depression: Efficiency of acute group treatment and booster sessions. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 272-279.
- Cunsolo Willox, A., Stephenson, E., Allen, J., Bourque, F., Drossos, A., Elgarøy, S.. . Wexler, L. (2015;2014;). Examining relationships between climate change and mental health in the circumpolar north. Regional Environmental Change, 15(1), 169-182. doi:10.1007/s10113-014-0630-z
- Cunsolo W. A., Stephenson, E., Allen, J., Bourque, F., Drossos, A., Elgaroy, S., & Wexler, L. (2015). Examining relationships between climate change and mental health in the Circumpolar North. Regional Environmental Change, (1), 169.
- Deckers, L. (2010). Motivation. Boston, Mass.: Allyn & Bacon.
- Dogra, N., Srivastava, S., & Energy and Resources Institute. (2012). Climate change and disease dynamics in India.
- Edwards, B., Gray, M., & Hunter, B. (2014;2015;). The impact of drought on mental health in rural and regional australia. Social Indicators Research, 121(May 2014), Advance online publication-194. doi:10.1007/s11205-014-0638-2
- Egger, H. L., & Emde, R. N. (2011). Developmentally sensitive diagnostic criteria for mental health disorders in early childhood: The diagnostic and statistical manual of mental disorders-IV, the research diagnostic criteria-preschool age, and the diagnostic classification of mental health and developmental disorders of infancy and early childhood-revised. American Psychologist, 66(2), 95-106. doi:10.1037/a0021026
- Felix, E., Afifi, W., & Afifi, T. (2012). The impact of uncertainty and communal coping on mental health following natural disasters. Anxiety, Stress & Coping, 25(3), 329-347. doi:10.1080/10615806.2011.603048
- Fernandes, T. (2013). Mental health. Nursing Standard, 27(30), 58.
- Friedrich, M. J. (2010). Treating mental health disorders. Jama, 304(19), 2116-2116. doi:10.1001/jama.2010.1670
- Galambos, C. M. (2005). Natural disasters: Health and mental health considerations. Health and Social Work, 30(2), 83-86.
- Ghatge, N., & Rasal, O. (2013). Climate Change: Causes‚ Consequences and Coping Strategies. Palhar Nagar: International E Publication.
- Hansen, A., Bi, P., Nitschke, M., Ryan, P., Pisaniello, D., & Tucker, G. (2008). The effect of heat waves on mental health in a temperate australian city. Environmental Health Perspectives, 116(10), 1369-1375. doi:10.1289/ehp.11339
- Harper, F. D., Harper, J. A., & Stills, A. B. (2003). Counseling children in crisis based on maslow's hierarchy of basic needs. International Journal for the Advancement of Counselling, 25(1), 11-25. doi:10.1023/A:1024972027124
- Hofmeijer, I., Ford, J. D., Berrang-Ford, L., Zavaleta, C., Carcamo, C., Llanos, E.. . Namanya, D. (2013;2012;). Community vulnerability to the health effects of climate change among indigenous populations in the peruvian amazon: A case study from panaillo and nuevo progreso. Mitigation and Adaptation Strategies for Global Change, 18(7), 957-978. doi:10.1007/s11027-012-9402-6
- Klerman, G. L., Weissman, M. M., Rounsaville, B., & Chevron, E. (1984). Interpersonal psychotherapy of depression. New York: Basic Books.
- Kokai, M., Fujii, S., Shinfuku, N., & Edwards, G. (2004). Natural disaster and mental health in asia. Psychiatry and Clinical Neurosciences, 58(2), 110-116. doi:10.1111/j.1440-1819.2003.01203.x
- Kronlid, D. (2014). Climate Change Adaptation and Human Capabilities: Justice and Ethics in Research and Policy. New York, NY: Palgrave Macmillan.
- Marks, I., Shaw, S., & Parkin, R. (1998). Computer-aided treatments of mental health problems. Clinical Psychology: Science and Practice, 5(2), 151-170. doi:10.1111/j.1468-2850.1998.tb00141.x
- McFarlane, A. C., & Van Hooff, M. (2013). Impact of childhood exposure to a natural disaster on adult mental health : 20-year longitudinal follow-up study. British Journal of Psychiatry, 203(6), 409-416.
- OBrien, L. V., Berry, H. L., Coleman, C., & Hanigan, I. C. (2014). Drought as a mental health exposure. Environmental Research, 131, 181-187. doi:10.1016/j.envres.2014.03.014
- Padhy, S. K., Sarkar, S., Panigrahi, M., & Paul, S. (2015). Mental health effects of climate change. Indian Journal of Occupational and Environmental Medicine, 19(1), 3. doi:10.4103/0019-5278.156997
- Pearce, M., Eagle, L., Low, D., & Schurmann, A. (2015). CUT FROM 'COUNTRY': THE IMPACT OF CLIMATE CHANGE ON THE MENTAL HEALTH OF ABORIGINAL PASTORALISTS. Australasian Journal Of Regional Studies, 21(1), 50-79.
- Psychiatry changes.(diagnostic and statistical manual of mental disorders). (2010). Nature, 463(7283), 854.
- Rafique, I. (2013). Mental health. Pakistan Journal of Medical Research, 52(4), 95.
- Reifels, L., Naccarella, L., Blashki, G., & Pirkis, J. (2014). Examining disaster mental health workforce capacity. Psychiatry, 77(2), 199.
- Riasat, R. (2013). Mental wellbeing in the workplace for GPs. Innovait, 6(9), 570-578.
- Schlesinger, W. H. (2011). Climate change. Interpretation, 65(4), 378
- Sharma, M., Atri, A., & Branscum, P. (2013). Foundations of mental health promotion. Burlington, MA: Jones & Bartlett Learning.
- Singh, A., & Purohit, B. M. (2014). Public Health Impacts of Global Warming and Climate Change. Peace Review, 26(1), 112-120.
- Tannock, R. (2013). Rethinking ADHD and LD in DSM-5: Proposed changes in diagnostic criteria. Journal of Learning Disabilities, 46(1), 5-25. doi:10.1177/0022219412464341
- Taormina, R. J., & Gao, J. H. (2013). Maslow and the motivation hierarchy: Measuring satisfaction of the needs. The American Journal of Psychology, 126(2), 155-177. doi:10.5406/amerjpsyc.126.2.0155
- Thomas, F., Sabel, C. E., Morton, K., Hiscock, R., & Depledge, M. H. (2014). Extended impacts of climate change on health and wellbeing. Environmental Science And Policy, 44271-278.
- Tibbetts, J. H. (2015). Air quality and climate change: A delicate balance. Environmental Health Perspectives, 123(6), A148.
- Wang, X., Lavigne, E., Ouellette-kuntz, H., & Chen, B. E. (2014). Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in toronto, canada. Journal of Affective Disorders, 155, 154-161. doi:10.1016/j.jad.2013.10.042
- Watkiss, P., & Hunt, A. (2012;2011;). Projection of economic impacts of climate change in sectors of europe based on bottom up analysis: Human health. Climatic Change, 112(1), 101-126. doi:10.1007/s10584-011-0342-z
- Weissbecker, I. (2011). Climate change and human well-being: Global challenges and opportunities. New York: Springer.
