Motivation and emotion/Book/2016/Antidepressants and emotion
What are the effects of popular antidepressants on human emotions?
Overview
[edit | edit source]|
"it was really alarming at first, since the change was subtle, but I did notice that my surrounding took on a different tone at certain times: the shadows of nightfall seemed more somber, my mornings were less buoyant, walks in the woods became less zestful, and there was a moment during my working hours in the late afternoon when a kind of panic and anxiety overtook me..." - William Styron, Darkness Visible |

The emotional hold of depression, the overpowering feelings of anxiety, worthlessness, anger, aggression and guilt have long been studied in attempts to help people regain control over their lives. Antidepressants offer a way out of the constant battle with ones emotions and neurological studies have offered a biological basis for emotional disturbances. Understanding these processes are essential for rehabilitation and the limitations of the usefulness of antidepressants in emotion regulation must also be recognised to prevent relapses or false hope of the treatment.
The following chapter will explore the different types of antidepressants and their neural mechanisms. The effects of these treatments on emotions will also be looked at in relation to their long term and short term benefits. In addition, the limitations of emotional control with the use of antidepressants, such as 'blunted effects,' will also be evaluated.
Depression
[edit | edit source]Depression is a psychological mood disorder and people who suffer from it experience persistent feelings of sadness, hopelessness, worthlessness, guilt and loss of motivation or interest. Depression effects peoples thoughts, feelings, and other behaviours such as eating, drinking and sleeping. There are many interpretations of the underlying mechanisms of depression including the behaviourist theory, psychodynamic theory, cognitive approach theory, and humanist approach theory. According to these, depression can result from interactions within our environment, biological processes and cognitive dispositions.
Take an Online Depression, Anxiety and Stress Test (DAS) - Please note this is not a diagnostic tool, only a psychologist can properly diagnose depressive disorders.
Emotion
[edit | edit source]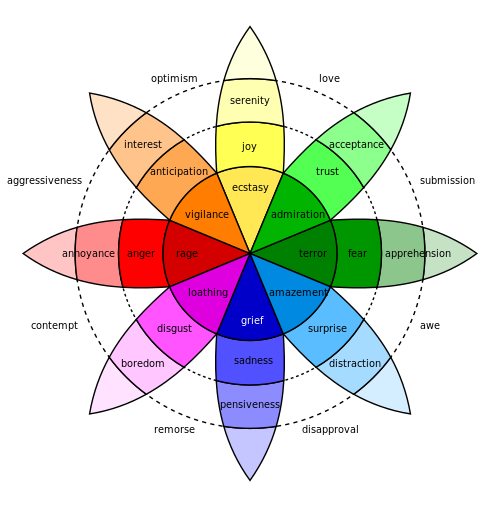
Emotions are short lived and help us to adapt to opportunities and challenges within our environment. They have synchronized brain activity that influences feelings, bodily responses, purpose, and expression. Emotion also plays a role in motivation as it directs and energizes behavior towards specific goals and is an indicator of how well or how poorly one is adapting to the constantly changing environment. The cause of an emotion stems from many interacting phenomenon such as significant life events, neural activity, cognitive processes, biological processes and feelings, sense of purpose, bodily arousal and social-expression.
Antidepressants
[edit | edit source]
Application
[edit | edit source]Antidepressants are used to treat depressive disorders and are most effective when used in combination with other psychosocial interventions. The main purpose of these drugs is to correct imbalances of neurotransmitters within the brain that are related to changes in emotion, mood and behaviours. The most common neurotransmitters associated with depression are serotonin, norepinephrine and dopamine.
Serotonin is commonly associated with the regulation of sleep, aggression, eating, sexual behaviour, and mood. Tryptophan is a precursor of serotonin and any deficiencies in the production of serotonin through these can lead to depressive symptoms (Neumeister, 2002). Antidepressants aim to reduce the effects of low serotonin levels by preventing the re-uptake of serotonin in the synapse (Neumeister, 2002). Serotonin re-uptake inhibition is one of the most common properties of antidepressants.
The role of norepinephrine is to help our bodies recognise and respond to stressful situations (Moret & Briley, 2011). It is thought that some people may suffer from deficiencies of norepinephrine, resulting in the inability to tolerate stress-induced depressive behaviour (Moret & Briley, 2011). Modifying the norepinephrine system to increase norepinephrine neurotransmissions has shown to be effective in treating emotional and cognitive symptoms of depression, while manipulations to decrease norepinephrine increases chances of depressive relapses (Moret & Briley, 2011).
Dopamine is an important neurotransmitter for the regulation of individuals motivation to seek out rewards (Rampello et al., 2000). It is also associated with feelings of pleasure and a lack of dopamine can result in depression associated with low motivation and energy for life (Rampello et al., 2000). Serotonin enhances dopamine outflow from neurones and therefore antidepressants such as serotonin re-uptake inhibitors are effective for increasing dopamine release (Rampello et al., 2000).
Neural mechanisms of antidepressants
[edit | edit source]
Neurotransmitters within the brain are used to communicate messages from one neuron to another. Neurotransmitters are housed in vesicles in the presynaptic neuron and are released into the synaptic gap between the presynaptic and postsynaptic neurone (Olijslagers et al., 2006). Receptors of the postsynaptic neuron bind with specific neurotransmitters and are activated. Once the message is received, the postsynaptic receptor releases the neurotransmitter back into the synapse where it can be taken up again by the presynaptic neuron through a process called re-uptake. The neurotransmitters are then repackaged and reused.
People with neurotransmitter deficiencies release less neurotransmitters into the synapse and, due to premature re-uptake, less are attached to their receptor molecules on the postsynaptic neuron. Antidepressant drugs work by blocking the re-uptake channels of neurotransmitters which increases the amount of neurotransmitters in the synapse available for attachment to receptor molecules (Olijslagers et al., 2006). In effect, depressive symptoms associated with low neurotransmitter levels is relieved.
Youtube video on how antidepressants work
Common types of antidepressants
[edit | edit source]
SSRIs are the most widely prescribed antidepressant drug in the current treatment for depression (Harmer, 2008). The drug includes fluvoxamine, fluoxetine, citaloprma, escitalopram, sertraline and paroxetine and is effective for treating symptoms of depression and anxiety (Gunnell et al., 2005). SSRIs are serotonin specific and only influence serotonin and not other neurotransmitters such as norepinephrine and dopamine (Gunnell et al., 2005). SSRIs also have less negative side effects compared to other types of antidepressants.
SNRIs are made up of duloxetine, venlafaxine and desvenlafaxine and is less popular then SSRIs. They prevent the reuptake of serotonin and norepinephrine by inhibiting the serotonin transporter (SERT) and the norepinephrine transporter (NET) (Dell'Osso et al., 2010). This drug may be more beneficial in treating a wider range of symptoms associated with depression due to this dual action (Dell'Oosso et al., 2010).
TCAs are made up of amitriptyline, nortiptyline, clomipramine, dothiepin, doxepin, imipramine and trimipramine. This antidepressant has more severe side effects than SSRIs but is used to treat treatment-resistant depressions (Anderson, 1998). TCAs block serotonin and norepinephrine re-uptake and also prevent action of acetylcholine.
MAOIs inhibit the action of monoamine oxidase which is a type of enzyme found in the brain that breaks down neurotransmitters such as serotonin (Volz & Gleiter, 1998). Like SSRIs, it increases serotonin levels and is used only if SSRIs were unsuccessful (Volz & Gleiter, 1998). The active components in this drug includes phenelzine and tranylcypromine.
Test your knowledge
[edit | edit source]|
|
How do antidepressants affect emotion?
[edit | edit source]
Tryptophan and low serotonin levels
[edit | edit source]Serotonin levels in the brain relies on the activity and availability of its precursor amino acid (tryptophan) (Harmer, 2008). The relationship between low serotonin levels and emotional processes have been studied with the administration of amino acid mixtures which decrease the availability of tryptophan in the brain (Reilly et al., 1997). Low tryptophan levels have been found to lower mood in recovered depressed patients (Ruhe et al., 2007), and has been linked to a reduction in the processing of positive versus negative affective emotional information (Harmer, 2008). A study by Murphy et al. (2002) tested this and found that a reduction in tryptophan levels slowed responses to positive verbal stimuli in an affective go-no go task. In addition, patients with lower availability of tryptophan also experienced a reduction in memory for positive affective information (Klaasen et al., 2002) and had increased interference for negative stimuli in a Stroop experiment by Evers et al. (2006). These reductions of positive biases have been linked to increased neural activity in the ventromedial prefrontal and sub-cortical areas (Roiser et al., 2007) (7) which is similar to the neural activity found in clinically depressed patients (Elliott et al., 2002). In light of these findings, it has been suggested that low serotonin levels due to decreased availability of tryptophan, factors associated with depression, is related to disturbances in the processing of emotional material (Harmer, 2008).
Repeated SSRI treatment
[edit | edit source]A study conduced by Harmer et al. (2004) found that after 7 days of continued SSRI administration patients were more inclined to see ambiguous facial expressions as happy. He also found that patients were able to memorise positive personality adjectives more accurately. Other studies have supported these findings and found reductions in threat-relevant processing after continued SSRI administration (Harmer et al., 2004). In particular, perceptions of disgusted, angry and fearful facial expressions were seen to reduce along with an increase in mood. Function resonance imaging studies have also found neural activity consistent with emotional changes during treatment. Reductions in amygdala, medial prefrontal, and fusiform responses to facial expressions eliciting fear and increases in fusiform responses to happy facial expressions were observed (Norbury et al., 2007). SSRI treatment also improved coupling between the amygdala, prefrontal cortex, striatum, and thalamus which are important neural networks associated with depression (Chen et al., 2007). fMRI data suggests that SSRI affects autonomic evaluation of emotional stimuli and also attentional processing (Harmer, 2008). Antidepressants appears then to have the ability to reduce emotional processing for negative stimuli and increase emotional processing for positive stimuli (Harmer et al., 2004). However, similar beneficial effects on emotional processing may not be seen with acute administration of antidepressant drugs (Harmer, 2008).
Long term effects versus short term effects of antidepressant administration
[edit | edit source]
The initial stages of treatment may increase emotional responses to threat related stimuli and anxiety levels may not decrease immediately (Harmer, 2008). Long term benefits of treatment are due to the downstream neuro-adaptive effects (Harmer, 2008). These include desensitisation of auto-receptors and down-regulation of postsynaptic serotonin receptors (Harmer, 2008). It is also theorised that the delay in the effectiveness of antidepressants is due to postponed expression of cellular action (Harmer, 2008). Another explanation may also be that antidepressants are not direct mood enhancers but rather affect the mechanisms of processing emotional stimuli, which only has beneficial consequences over time (Harmer, 2008). In accordance with this view, antidepressants have a bottom-up effect, and new life experiences are associated with a more positive bias which leads to improved mood (Harmer, 2008). Therefore, improvements in emotion may be linked to re-learning emotional associations (Harmer, 2008). The concept of re-learning has been thought to be associated with antidepressant induced synaptic plasticity (Manji et al., 2003).
Blunted emotions
[edit | edit source]In some cases, patients taking antidepressants report blunted and limited emotional responses (Price, Cole, & Goodwin, 2009). A study conducted by Price et al. (2009) investigated the experiences of blunted emotions in patients taking SSRIs. The study found that people experienced less intense emotions after the administration of SSRIs and that all their emotions seemed 'dulled', 'numbed', or 'flattened.' Some patients even reported feeling no emotion at all during treatment (Price, Cole, & Goodwin, 2009). Patients were however able to recognise and respond to emotional cues appropriately and had full control over there emotions (Price, Cole, & Goodwin, 2009). Positive emotions were reduced by most patients whereas negative emotions were reduced by all patients, the latter being more beneficial and outweighing the negative effect on positive emotions (Price, Cole, & Goodwin, 2009). Emotional detachment was also experienced by most patients and they described it as feeling as if they were in a 'limbo' of 'unreality' (Price, Cole, & Goodwin, 2009). These feelings were associated with emotional detachment from family, friends and partners (Price, Cole, & Goodwin, 2009). Another consequence of antidepressant treatment was that patients reported feelings of not caring for themselves or others and a loss of self-identity (Price, Cole, & Goodwin, 2009).
Conclusion
[edit | edit source]Antidepressants have many beneficial aspects in the regulation of emotions to help improve the quality of life for those suffering from depression. It is possible that people using these medications adapt to form more positive schemas and biases. There are some possible negative side effects of the treatment, such as early increases in anxiety and blunted emotions which may negatively impact individuals. The chapter has briefly covered the major effects of antidepressants on emotions however, a much broader scope exists. The differences between treatments for their effects on emotion has not yet been determined and may be a useful topic for further research in this field.
See also
[edit | edit source]Depression and motivation (Book Chapter, 2010)
Depression and motivation (Book Chapter, 2014)
Self-esteem and depression (Book Chapter, 2014)
Depression in older adults (Book Chpater, 2015)
Trans-cranial direct current stimulation and depression (Book Chapter, 2015)
Depression in adolescence (Book Chapter, 2015)
Norepinephrine and emotional disorders (Book Chapter, 2015)
References
[edit | edit source]Chen, C. H., Suckling, J., Ooi , C., Fu , C. H., Williams, S. C., & Walsh , N. D. (2007). Functional coupling of the anygdala in depressed patients treated with anti-depressant medication.
Dell'Osso, B., Buoli, M., Baldwin, D. S., & Altamura, A. (2010). Serotonin norepinephrine reuptake inhibitors (SNRIs) in anxiety disorders: a comprehensive review of their clinical efficacy. Human Psychopharmacology: Clinical and Experimental, 25(1), 17-29.
Elliott, R., Rubinsztein, J. S., Sahakian, B. J., & Dolan , R. J. (2002). The neural basis of mood-congruent processing biases in depression . Psychiatry, 59, 597-604.
Evers, E. A., van derVeen, F. M., Jolles, J., Deutz , N. E., & Schmitt, J. A. (2006). Acute tryptophan depletion improves performance and modulates the BOLD response during a Stroop task in healthy females. Neuroimage, 32, 248-255.
Gunnell, D., Saperia, J., & Ashby, D. (2005). Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA's safety review. Bmj, 330(7488), 385.
Harmer , C. J. (2008). Serotonin and emotional processing: Does it help explain antidepressant drug action? Neurophramacology , 55, 1023-1028.
Harmer, C. J., Shelley, N. C., Cowen, P. J., Cowen , P. J., & Goodwin , G. M. (2004). Increased positive versus negative affective perception and memory in healthy volunteers following selective serotonin and norepinephrine reuptake inhibition. American Journal of Pscyhiatry, 161, 1256-1263.
Klaassen, T., Riedel, W. J., Deutz , N. E., & van Praag, H. M. (2002). Mood congruent memory bias induced by tryptophan depletion . Psychology Medicine, 32, 167-172.
Manji, H. K., Quiroz, J. A., Sporn, J., Payne , J. L., Denicoff, K., & Gray, A. (2003). Enhancing neuronal plasticity and cellular resilience to develop novel, im-proved therapeutics for difficult-te-treat depression . Psychiatry , 53, 707-742.
Moret, C., & Briley, M. (2011). The importance of norepinephrine in depression. Neuropsychiatr Dis Treat, 7(Suppl 1), 9-13.
Murphy, F. C., Smith, K. A., Cowen, P. J., Robbins, T. W., & Sahakian , B. J. (2002). The effects of tryptophan depletion on cognitive and affective processing in healthy volunteers. Psychopharmacology, 163, 42-53.
Neumeister, A. (2002). Tryptophan depletion, serotonin, and depression: where do we stand?. Psychopharmacology bulletin, 37(4), 99-115.
Norbury, R., Mackay, C. E., Cowen, P. J., Goodwin , G. M., & Harmer, C. J. (2007). Short-term antidepressant treatment and facial processing. Functional magnetic resonance imaging study. Journal of Psychiatry, 190, 531-532.
Olijslagers, J. E., Werkman, T. R., McCreary, A. C., Kruse, C. G., & Wadman, W. J. (2006). Modulation of midbrain dopamine neurotransmission by serotonin, a versatile interaction between neurotransmitters and significance for antipsychotic drug action. Current neuropharmacology, 4(1), 59-68.
Price , J., Cole , V., & Goodwin, G. M. (2009). Emotional side-effects of selective serotonin reuptake inhibitors: qualitative study. The British Journal of Psychiatry, 195(3), 211-217.
Rampello, L., Nicoletti, F., & Nicoletti, F. (2000). Dopamine and depression. CNS drugs, 13(1), 35-45.
Reilly, J. G., McTavish, S. F., & Young, A. H. (1997). Rapid depletion of plasma tryptophan: a review of studies and experimental methodology. Journal of Pscyhopharmacol, 11(4), 381-392.
Roiser, J. P., Levy , J., Fromm, S. J., Wang, H., Hasler, G., & Sahakian, B. J. (2007). The effect of acute tryptophan depletion on the neural correlates of emotional processing in healthy volunteers. Neuropsychopharmacology, 10, 449-461.
Ruhe, H. G., Mason, N. S., & Schene, A. H. (2007). Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of mono-amine depletion studies. Psychiatry, 12(4), 331-359.
Volz, H. P., & Gleiter, C. H. (1998). Monoamine oxidase inhibitors. Drugs & aging, 13(5), 341-355.
External links
[edit | edit source]Depression, Anxiety and Stress test
- Resources needing improved grammar
- Resources needing facts checked
- Resources needing clarification
- Resources needing rewritten
- Resources needing spell checking
- Resources needing clarification by what
- Motivation and emotion/Book/2016
- Motivation and emotion/Book/Depression
- Motivation and emotion/Book/Drugs/Antidepressants
