Upper Limb Orthotics/Distal Radial Fracture
Describe your case study
[edit | edit source]- The patient is a 23 year old female basketball player who suffered a fracture to her right wrist during a game. Her injury was sustained as another player bumped into her and she fell on an outstretched hand, resulting in an undisplaced, distal radial fracture.
- She has presented to us three weeks after her injury, so far having a closed reduction and been in plaster casts during the first three weeks of her treatment.
- The patient is hoping for a fast recovery and a device that will allow her to still complete self-care activities as well as continue some training activities in and easy and hygienic manner.
Written information
[edit | edit source]Evidence
[edit | edit source]Distal radial fractures are the most common fractures seen in emergency departments Kennedy and Hanel (2013) with statistics showing that up to two hundred thousand fractures a year that of the distal radius (Liporace, Adams, Capo, & Koval, 2009) and up to 20% of all fractures attended to involving the distal aspect of the radius in the United States, every year (P. M. Simic & A. J. Weiland, 2003). There are two main groups that are most frequently seen in these emergency rooms are; young adults aged between eighteen and twenty-five years of age, who sustain their injuries through sports or motor vehicle accidents, and adults over the age of sixty-five caused by falls and fragile bones (Voda, 2011). The high incidence of this injury may be better understood once the anatomy and function of the bone is further discussed.
The radius is one of the two long bones that make up the forearm and it is positioned laterally when observing the arm in anatomical position. It is thin proximally and wide distally, which explains its large contribution to the wrist joint and its role in movement of the hand (Marieb & Hoehn, 2007). This joint articulation describes why the long bone has “three concave articular surfaces- the scaphoid fossa, the lunate fossa and the sigmoid notch” and furthermore, why a distal fracture of this bone is often referred to as a wrist fracture (Paul M Simic & Andrew J Weiland, 2003). Paul M Simic and Andrew J Weiland (2003) also state that at the metaphyseal flare of the radius, there is an increase in cancellous bone and decrease in the corticol bone, which results in a segment of the bone being more inclined to fracture, especially as it plays a large role in wrist motion and load transmission. Although the muscles of the forearm are not directly impacted by this injury, they do control the movements in this region which one may wish to prevent throughout the healing process of the fracture. Marieb and Hoehn (2007) displays how the muscles of the forearm are separated into two groups; the anterior muscles and the posterior compartments, with each group responsible for a general function, the anterior group known as the flexors which includes two pronator muscles, and the posterior, as the extensors, which includes a supinator muscle . The healing process of a fracture relies heavily on the blood supply to the fractured region, and Lamas et al. (2009) not only found that the distal radius relies on the “radial, ulnar, anterior interosseus and posterior interosseus arteries”, but that throughout the healing of non-displaced and closed fractures, the medullary circulation remains dominant. Walsh (2013) discusses the many factors that determine the type of fracture that results from falling on an outstretched hand (also known as FOOSH), and the impact that they can have on the fracture pattern. These factors include; the patient’s mass, the ulna and radius’ degree of deviation, and the extent of wrist flexion or extension at the time, which will all cumulatively determine the impact that the energy forces will have when going through the distal ends of the long bones. This variance in fracture patterns calls for a particular classification system that will allow clinicians to differentiate between the severity of fractures in a detailed manner as well as identify relative treatment options, and Paul M Simic and Andrew J Weiland (2003) and (Hanel, Jones, & Trumble, 2002) describe the AO classification system to be very “detailed”. The AO classification breaks down fractures of long bones into three categories; extra-articular, partial articular and complete articular, and these groups are furthered narrowed into subgroups based on the characteristics that the particular fracture presents.
According to Muller’s system, our client presents with a 23 A2.1 fracture which is defined as an non-displaced extra articular fracture of the metaphysis, involving neither the radiocarpal nor distal radioulnar joints and exhibits no abnormal palmar or dorsal tilt (Müller, Koch, Nazarian, & Schatzker, 1990). (Liporace et al., 2009) identified a non-displaced distal radial fracture as “4-mm overall shortening, less than 5-mm decrease in radial height, less than 10° change in volar tilt from the contralateral extremity, and less than 50% dorsal comminution”, which is what our client presents with. Before any treatment options can be considered for the management of the distal radial fracture, the nature of the fracture as well as the individual’s activity level must be established in order to determine whether closed, or open reduction will be performed (Voda, 2011). Closed reduction, also known as anatomical alignment of a fracture, is a common option for non-displaced and non-articulated fractures (Voda, 2011), and once this has been performed and it has been established that there has been no further displacement, orthotic management can be considered.
Orthotic Treatment Options
[edit | edit source]The treatment of distal radial fractures is a very controversial topic as there is no single and definitive treatment that has been agreed upon and consistently used (ALTISSIMI, ANTENUCCI, FIACCA, & MANCINI, 1986); (Hanel et al., 2002) and this is most likely due to the fact that there is not enough evidence to determine the best treatment options (Handoll, Madhok, & Howe, 2006). Typically, plaster casting is commonly used from one to three weeks following the reduction or surgery of a wrist fracture, and subsequently, an orthotic device is prescribed after the initial period healing period (ALTISSIMI et al., 1986; Hanel et al., 2002). The role of an orthotic intervention for a fracture is to ensure that it immobilises the effected region whilst still maintaining function (Walsh, 2013).
A common device used to fulfil these requirements, is the sugar tong splint (Liporace et al., 2009) as it restricts forearm rotation, which is recommended for distal radial fracture recovery (Kim, Kook, & Kim, 2012). Kim et al. (2012) used a prefabricated sugar tong splint with its trim lines being somewhat proximal metacarpophalangeal joint dorsally and extended around the proximal and distal radioulnar joint and held in place by a four inch elastic bandage. It was found through this investigation that “active supination and pronation had decreased to 31% and 34% of the value with no immobilisation,” (Kim et al., 2012) which when compared to the results of a short arm cast; 33% and 36% respectively, is not the most efficient. A short arm cast of this nature is generally worn from weeks three through to six according to Hanel et al. (2002), and is more appropriate for our client as it will allow her to perform more activities of daily living when compared to a sugar tong splint. This extra activity is allowed mainly due to the trim lines of the device, which are situated proximally to the metacarpophalangeal joints and distal to the radioulnar crease Kim et al. (2012). This ultimately allows more elbow flexion than the sugar tong splint and will avoid capsular contracture to allow metacarpophalangeal joint flexion (Müller et al., 1990). Distal radial fractures of this nature are typically positioned in most devices with the forearm supinated to prevent the tugging of the brachioradialus, and with the wrist in a neutral position throughout the treatment process Hanel et al. (2002) which is what our client presents with in her initial plaster cast.
Orthotic Treatment vs Surgical Intervention
[edit | edit source]Egol, Walsh, Romo-Cardoso, Dorsky, and Paksima (2010) state that it is imperative that a surgeon assess the risks, benefits and alternatives to any treatment when dealing with a fracture and ultimately choose what is best for the patient. Surgical intervention is often seeked when treating unstable distal radial fractures (Driessens et al., 2013) or in high energy injuries (Hanel et al., 2002) in the form of open reduction internal fixation (ORIF). ORIF has become more popular over the years, especially with the introduction of the volar locking plate as it is said that this internal fixation will allow immediate range of motion of the wrist, whilst ensuring that the correct anatomical alignment of the radius in maintained throughout this speedy healing process (Rozental et al., 2009). One factor that must be considered when contemplating ORIF, is the risk of superficial or deep infection at the fracture site, but based on results from an investigation conducted by Tan, Beredjiklian, and Weiland (2005), the chances of infections occuring are slim.
When taking into consideration all of the factors involved and discussed with relation to our patients fracture and goals, it is recommended that she have a short arm cast fabricated to ensure that she experiences a healthy recovery that accomodates for her needs.
References
[edit | edit source]ALTISSIMI, M., ANTENUCCI, R., FIACCA, C., & MANCINI, G. B. (1986). Long-term results of conservative treatment of fractures of the distal radius. Clinical orthopaedics and related research, 206, 202-210.
Driessens, S., Diserens-Chew, T., Burton, C., Lassig, E., Hartley, C., & McPhail Bphty, S. (2013). A retrospective cohort investigation of active range of motion within one week of open reduction and internal fixation of distal radius fractures. Journal of Hand Therapy, 26(3), 225-231. doi: 10.1016/j.jht.2013.05.002
Egol, K., Walsh, M., Romo-Cardoso, S., Dorsky, S., & Paksima, N. (2010). Distal radial fractures in the elderly: operative compared with nonoperative treatment. The Journal of Bone & Joint Surgery, 92(9), 1851-1857.
Handoll, H., Madhok, R., & Howe, T. (2006). Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev, 3.
Hanel, D. P., Jones, M. D., & Trumble, T. E. (2002). Wrist fractures. Orthopedic Clinics of North America, 33(1), 35-57.
Kennedy, S. A., & Hanel, D. P. (2013). Complex distal radius fractures. Orthopedic Clinics of North America, 44(1), 81-92. doi: 10.1016/j.ocl.2012.08.008
Kim, J. K., Kook, S. H., & Kim, Y. K. (2012). Comparison of forearm rotation allowed by different types of upper extremity immobilization. Journal of Bone & Joint Surgery, American Volume, 94(5), 455-460.
Lamas, C., Llusà, M., Méndez, A., Proubasta, I., Carrera, A., & Forcada, P. (2009). Intraosseous vascularity of the distal radius: anatomy and clinical implications in distal radius fractures. Hand, 4(4), 418-423.
Liporace, F. A., Adams, M. R., Capo, J. T., & Koval, K. J. (2009). Distal radius fractures. Journal of orthopaedic trauma, 23(10), 739-748.
Marieb, E. N., & Hoehn, K. (2007). Human anatomy & physiology: Pearson Education.
Müller, M. E., Koch, P., Nazarian, S., & Schatzker, J. (1990). The comprehensive classification of fractures of long bones: Springer-Verlag Berlin.
Rozental, T. D., Blazar, P. E., Franko, O. I., Chacko, A. T., Earp, B. E., & Day, C. S. (2009). Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. Journal of Bone & Joint Surgery, American Volume, 91(8), 1837-1846. doi: 10.2106/JBJS.H.01478
Simic, P. M., & Weiland, A. J. (2003). Fractures of the distal aspect of the radius: changes in treatment over the past two decades. Journal of Bone & Joint Surgery, American Volume, 85A(3), 552-564.
Tan, V., Beredjiklian, P. K., & Weiland, A. J. (2005). Intra-articular fractures of the hand: treatment by open reduction and internal fixation. Journal of orthopaedic trauma, 19(8), 518-523.
Voda, S. C. (2011). Bad breaks: A nurse's guide to distal radius fractures. Nursing, 41(8), 34-41. doi: 10.1097/01.NURSE.0000399599.97411.cb
Walsh, C. R. (2013). Wrist fractures in adults: Getting a grip. Nursing, 43(4), 38-46. doi: 10.1097/01.NURSE.0000427986.39188.a6
Search Stratergy
[edit | edit source]The databases used were CINAHL, Cochrane and Google Scholar. The key search terms used for the research of this topic were: distal radial fractures AND bracing, wrist fractures, non-displaced wrist fracture AND surgery, wrist fracture bracing and radial anatomy. The results found a combination of recent and dated studies, but the information extraculated was deemed most appropriate and relevant.
Functional Aims and Goals
[edit | edit source]The functional aims and goals for the Plaster of Paris (POP) cast and Low Temperature Thermoplastic (LTT) brace are very similar as the primary function for each device is to immobilise any movement at the wrist joint in order to allow the distal radius to heal in its correct alignment. A POP cast has been used for the client during the first three weeks of treatment after closed reduction, as this method not only prevents range of motion at the wrist joint but can be replaced easily to accommodate for any fluctuation in limb size due to oedema. The required immobilisation is achieved by ensuring that the device is applied over the wrist joint and maintains a neutral position whilst avoiding any unnecessary immobilisation of other joints, and this is determined by the device trimelines. The proximal trimeline is approximately an inch and a half distal to the elbow joint, allowing for elbow flexion and extension. Finger opposition is also allowed with the distal trimline being just proximal to the distal palmar crease. Both devices cover the dorsal aspect of the outlined region as they must be removable for hygienic purposes as the client experiences excessive perspiration due to high activity levels. As a result of the devices not being circumferential, they both require suspension and this is where the two differ. The POP cast is suspended with bandages whereas the LTT orthosis is suspended with Velcro straps; both methods allowing for adjustments in size if necessary.
Design
[edit | edit source]Based on our client’s lifestyle- the device manufactured must be able to provide the necessary circumferential support to immobilise the wrist joint, but also be removal for hygienic maintenance of perspiration. To allow for this function and provide circumferential pressure, a piece of 260 density/3mm EVA has been attached with rivets to the lateral aspect of the device to enclose the dorsal aspect of the forearm into the device. This bivalve mechanism is secured with the use of adjustable Velcro straps to not only provide the required pressure, but also allow for any fluctuations in size of the limb. This will also ensure that the ideal position of a neutral wrist and forearm is maintained whilst still immobilising the wrist joint. The trimlines of the device should allow for functional movement of the fingers and elbow joint with the proximal trimline being approximately two inches distal to the elbow, and the distal trimline just proximal to the distal palmer crease. These trimlines should be contoured and designed to avoid any limitation of movement of other joints, as well as ensure that no pinching or of the soft tissue occurs. The edges of the distal trimline and the thumbhole are folded back to vanquish any sharp edges, as well as the proximal aspect of the device being slightly flared out.
-
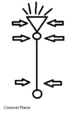
Force Diagram- Coronal Plane
-
Force Diagram- Sagittal Plane
-
Design- Coronal View
-
Design- Sagittal View
Manufacturing process
[edit | edit source]Step one-
• Trace your clients arm on a piece of paper with the pen directly vertical to the paper NOT pointed towards their arm
Step two-
• Mark all the anatomical landmarks such as the metacarpophalangeal (MCP) joint and interphalangeal joints of the thumb, the distal palmer crease and the wrist
• Draw a line down directly from the index finger and across from the MCP joint of the thumb and where these two points meet is the apex of the circle cut out for the thumb hole
Step three-
• Create the distal trimline by cutting straight across the distal palmer crease and outline approximately two inches around the arm
• Fan out the width along the proximal trimline to allow for the soft tissue in this region
• Cut out thumb hole
Step four
• Try on client and take note of any adjustments that may need to be made
Step five
• Outline design onto material accommodating for any of the changes that need to be made
Step six-
• Cut out roughly around the design using shears
Step seven-
• Place into frypan with water at 60 degrees Celsius
• Push plastic under water using scissors
• Whilst the plastic is softening, prepare your client by positioning them with elbow support, neutral forearm and wrist and a slightly opposed thumb
• Once plastic is soft enough take out with care and dry on towel
Step eight-
• Cut plastic around the design whilst it is still soft
Step nine-
• Align the proximal and distal ends of the plastic against the clients forearm
• Secure it by folding the onto the arm and pinching the edges in place
• Fold edges of the distal trimline and the thumb hole away from client
• Mould to patients forearm whilst still maintaining the neutral position and smoothing away any potential air pockets
Step ten-
• Measure how much of the dorsal aspect of the forearm has to be covered by the EVA and cut out appropriate whilst considering approximately 1.5 cm for attachment
Step eleven-
• Taper the lateral edges of the EVA to prevent any discomfort for the client
• Grind on an angle
Step twelve-
• Place the EVA in the oven until softened
• Mould to patients arm to get some conformity
Step thirteen-
• Use rivet punch to place appropriate holes in the lateral aspect of the device and be sure to place them in between the desired strap locations and not underneath
• Place appropriate sized rivet head and body in punched holes
Step fourteen-
• Firmly secure rivets and EVA
Step fifteen-
• Cut Velcro loop straps and sticky back hook
Step sixteen-
• Heat the orthoses on the lateral aspect just above the thumb hole and heat the loop then attach the two to ensure a firm attachment
Step seventeen-
• Place the sticky back hook Velcro on volar aspect at the proximal edge of the device, the wrist joint, and laterally at the distal point
-
Step One
-
Step Two
-
Step Three
-
Step Four
-
Step Five
-
Step Six
-
Step Seven
-
Step Eight
-
Step Ten
-
Step Eleven
-
Step Twelve
-
Step Thirteen
-
Step Fourteen
-
Step Fifteen
-
Step Sixteen
-
Step Seventeen
Critique of fit
[edit | edit source]The patient is a twenty-three year old female basketball player who suffered a fracture to her right wrist during a game. She has presented three weeks after sustaining her undisplaced distal radial fracture and has so far been managed with a closed reduction and immobilization in a plaster cast.
On presentation, the client reported with a throbbing pain and extreme loss of function in her right wrist. The client aims to be able to resume her usual activities and physical training whilst allowing her fracture to heal with reduced pain. Due to the client’s desire to continue training during her management, hygiene must be taken into consideration when designing the prescribed orthosis.
A physical assessment was completed and revealed restricted movement of the wrist joint as well as oedema. All of the surrounding joints presented with normal ranges of motion and no restrictions.
The goal of the orthotic management is to not only achieve the clients goals to the greatest of our ability, but to do so whilst preventing any displacement and malalignment of the long bone during the healing process.
In order to achieve these goals, an orthotic prescription has been developed to immobilize the wrist joint in a neutral position within a circumferential device. The orthosis must not only distribute the applied pressure over throughout the forearm and wrist joint by extending the lever arm of the straps, and ensuring that the straps are adjustable to accommodate for any fluctuations in limb size.
The device must also be removable and easy to maintain hygienically, so the bivalve orthosis is manufactured out of low temperature thermoplastic and ethyl vinyl acetate. The surrounding joints must not be restricted and in order to achieve this, the proximal trimline is approximately an inch distal to the cubital fossa to allow elbow flexion and extension, and the distal is just proximal to the distal palmer crease allowing for full range of motion of the digits.
When assessing the fit of the design, the trimlines of the device are appropriate allowing the desired unrestricted movement of the surrounding joints of the wrist (refer to Figure 2). The three Velcro straps do allow for the an adjustable intimate fit as desired, but the most distal strap does sit slightly higher then the EVA which may result in some rubbing onto the dorsal aspect of the hand. This could have been avoided by slightly increasing the length of the EVA.
The angle of the brace is not optimal as it is in slight flexion and this would have occurred during the molding process with the client not maintaining the initially acquired position, that being of a neutral wrist joint (no flexion or extension).
Aesthetically the device does have has scuffs and trimline markings which could have been avoided by more carefully marking with an erasable marker. Folding of the plastic around the distal trimline and thumbhole could also be much tidier (refere to Figure 1).
-
Figure One
-
Figure Two
-
Figure Three
Outcome measures
[edit | edit source]Outcome measures have received a lot of attention in the scope of healthcare over recent years and this is not only due to the discrepancies in the evidence supporting current treatment methods but the costs the healthcare system incurs as a result (MacDermid, J. C. et al, 1998).
The Patient Rated Wrist Evaluation (PRWE) is fifteen-itemed questionnaire consisting of a pain and function subscale that is deemed to be an appropriate measure for fractures of the wrist and hand. There are five questions relating to pain and five relating to function and all questions are answered using a simple scale ranging from zero to ten. The scale is clearly defined and described for its application to all questions. Due to the simplicity of this questionnaire, it can be self administered or administered by a health care professional.
The PRWE states in a brief explanation, that the questions should be answered regarding the average difficulty the individual experiences over the course of a week. As our client has suffered a distal radial fracture, one of the key things that has been addressed during the management aside from immobilization of the joint, is reducing the pain involved with the injury. The pain scale of this questionnaire is predominantly subjective with it ranging from “no pain” to “worst ever”, which allows for quite a large range from one to ten for the patient to select from.
The functionality subscale of the PRWE also ranges from zero (no difficulty) to ten (unable to do), which allows for the patient to interpret these subjective levels. This is an important factor to consider when assessing the efficiency of a prescribed device, as it is vital that the trimlines of the design do not inhibit any functionality during management.
Due to the lack of function and pain involved with a fracture, the initial baseline measure could not be taken prior to the application of the prescribed device. Therefore, the baseline measure has been taken at four weeks post reduction and the following at eight weeks post reduction. The two attached files will demonstrate this.
When comparing the responses to the questionnaire, it is evident that there has been significant improvement in the patient’s pain and functionality with the device in use. There were a couple of questions left unanswered in the baseline measure, but the provided user manual clearly describes how to deal with such situations when assessing the results.
Although the PRWE has been designed to be used in association with measures such as radiographic assessment, it has been deemed to be an appropriate and simple measure to assess patient perceived disability (MacDermid, J. C. et al, 1998).
MacDermid, J. C., Turgeon, T., Richards, R. S., Beadle, M., & Roth, J. H. (1998). Patient rating of wrist pain and disability: a reliable and valid measurement tool. Journal of Orthopaedic trauma, 12(8), 577-586, doi: 0890-53390890-5339.