Upper Limb Orthotics/De Quervain's Tenosynovitis
Case study
[edit | edit source]A 35-year-old female piano teacher is presented with sharp pain and swelling along the radial side of her right wrist, which is her dominant hand. She states that the pain has been present for three weeks, often aggravated when lifting and carrying her infant. She has taken time off from work because the pain has made it difficult for her to move her thumb and wrist when playing the piano. Physical examination revealed swelling at the base of the right thumb, decreased range of motion of the wrist and limited thumb abduction and extension. She tested positive for pain over the radial styloid with Finkelstein’s test, which is a diagnostic test for DeQuervain’s Tenosynovitis. The treatment is aimed toward decreasing the swelling and wrist pain as well as restoring hand function. The patient's goals are to have no pain when lifting her child and to return to work as soon as possible.
Written Information
[edit | edit source]
Introduction
[edit | edit source]De Quervain’s tenosynovitis is a common painful wrist pathology, which causes difficulties in daily activities. This condition falls under the umbrella term “repetitive strain injury” which affects the thumb (Yassi, 1997). It occurs most often in individuals between the ages of 30 and 50 and is more common in women than men (Wolf, Sturdivant, & Owens, 2009).
Anatomy
[edit | edit source]De Quervain’s tenosynovitis affects two thumb tendons in the first dorsal compartment of the wrist, the abductor pollicus longus (APL) and the extensor pollicis brevis (EPB) (Moore, 1997). The APL and EPB muscles originate on the dorsum of the forearm and its tendons travel side by side along the radial border of the wrist and inserts into the thumb. These tendons allow abduction and extension of the thumb as well as assist with wrist deviation. In De Quervain’s tenosynovitis, it is believe that there is an inflammation of the APL and EPB tendons, however, other research suggests that it is a degeneration of the tendons or irritation and constriction of the synovial sheath surrounding the tendons at the distal radial styloid (Clarke, Lyall, Grant, & Matthewson, 1998; Kay, 2000; Muckart, 1964).
Etiology
[edit | edit source]The most common cause of De Quervain’s tenosynovitis is overuse or repetitive movements of the thumb in combination with wrist deviation, such as grasping, lifting and twisting (Howell, 2012; Ranney, Wells, & Moore, 1995). This places tension on the tendons of the thumb, which leads to thickening of the tendon’s synovial sheaths, narrowing of the fibro-osseous canal and consequently abnormal gliding of the APL and EPB tendons (Moore, 1997). Some activities that have been postulated as potential risk factors for De Quervain tenosynovitis include repeated typing, piano playing and texting (Ashurst, Turco, & Lieb, 2010; Ilyas, Ast, Schaffer, & Thoder, 2007; Sakai, 2002). It is also often associated with pregnancy and rheumatoid arthritis (Kay, 2000; Read, Hooper, & Davie, 2000).
Clinical Presentation
[edit | edit source]
The primary clinical presentations of De Quervain’s tenosynovitis are localised tenderness or swelling around the radial styloid and pain on the radial side of the wrist. The pain may occur suddenly or gradually and can radiate proximally into the forearm or distally into the thumb. Any motion of the wrist and thumb may aggravate this pain. Other clinical signs might include altered sensation over the radial side of the hand, decreased range of motion (ROM) of the thumb and reduced grip strength. Diagnosis for De Quervain’s tenosynovitis is usually concluded by a positive Finkelstein’s test. Finkelstein’s test is performed with the patient’s thumb clasped in his/her hand followed by ulnar deviation of the wrist. This maneuver creates tension of the APL and EPB tendons, reproducing significant pain at the radial styloid process located at the base of the thumb (Dawson & Mudgal, 2010; Kay, 2000).
Treatment
[edit | edit source]Goals of therapy for De Quervain’s tendosynovitis are to alleviate the pain and to improve mobility and function of the hand. There are multiple treatment options available for this condition, which includes splinting, corticosteroid injection, anti-inflammatory drugs and surgery.
Orthotic Treatment
[edit | edit source]Conventionally, one of the initial managements for De Quervain’s tendosynovitis is to wear a wrist-thumb static splint, which is a device that maintains the hand in one position and restricts wrist and thumb movements, for at least four to six weeks to improve symptoms (Weiss, Akelman, & Tabatabai, 1994). The splint immobilises the wrist and the thumb, which inhibit gliding of the injured APL and EPB tendons, and thus promote healing of the tendons and decrease associated pain (Moore, 1997). It also provides support for the wrist, protection for the thumb and refrains repetitive thumb movements that may aggravate the condition (Huang et al., 2006; Neumann & Bielefeld, 2003). There are several types of splints prescribed to immobilise and protect the wrist and the thumb. Most commonly used are custom-fitted wrist-thumb thermoplastic splints (Huang et al., 2006), prefabricated neoprene thumb splints (Jongprasitkula, Suputtitadaa, Kitisomprayoonkula, & Pintawirujb, 2011) and thumb plaster splint (Hart, Kleinert, & Lyons, 2005). Although the splints are made of different materials, results in pain reduction and strength improvement are similar in patients with De Quervain’s tendosynovitis (Jongprasitkula et al., 2011). The splint typically placed the wrist in slight extension with the thumb in slight flexion and palmar abduction while allowing other fingers to move freely for normal hand function and prevent hand stiffness (Hart et al., 2005). Splinting is generally beneficial for management when the condition is in its early stages where the symptoms are less severe (Lane, Boretz, & Stuchin, 2001).
Other Treatment Options
[edit | edit source]In many cases, splinting is used in conjunction with corticosteroid injections or nonsteroidal anti-inflammatory drugs (NSAIDs) for a faster recovery time with symptom improvements in about three weeks (Richie & Briner, 2003).
Corticosteroid injection into the tendons is used to reduce inflammation around the wrist and thumb as well as relieve pressure on the APL and EPB tendons. A non-randomised study that compared corticosteroid injections alone and with splint treatment found that there is a 57% success rate with splinting and corticosteroid injection together, 19% success rate with splinting alone and a 67% success rate with injection alone (Weiss, Akelman, & Tabatabai, 1994). Similarly, a single group experimental study demonstrated that injection treatment followed by splinting had a 62% success rate. A pooled quantitative literature review reported a higher cure rate (61%) for splinting with injection treatment, in comparison to a 14% cure rate for splinting alone (Richie & Briner, 2003). However, there are several potential side effects following corticosteroid injection. This include skin infection, skin depigmentation, tendon rupture and subcutaneous fat atrophy (Cardone & Tallia, 2002; Sampson, Wisch, & Badalamente, 1994).
NSAIDs can be administered orally to help ease inflammation of the APL and EBP tendons and reduce pain. A non-randomised study identified that wrist splints with NSAIDs were effective only in a small, but discrete, population of patients with mild symptoms. The relief of symptoms was diminished in patients with moderate to severe symptoms (Lane et al., 2001).
Surgery may be recommended if patients are unresponsive to conservative treatment and symptoms persist after four months (Harvey, Harvey, & Horsley, 1990). In surgical treatment, part of the tendon sheath is excised to decompress the APL and EPB tendons. It has been reported to be effective with a 91% cure rate. Although surgery may have high success rates and can enable patients to return to normal activities in two to three weeks, surgery is more costly, invasive and can be associated with more complications (Ta, Eidelman, & Thomson, 1999). De Quervain’s tenosynovitis can produce anatomical variations, making surgery more challenging to perform and succeed with (Alemohammad, Yazaki, Morris, Buford, & Viegas, 2009).
Summary
[edit | edit source]De Quervain’s tenosynovitis is a common wrist pathology. However, there is still a lack of evidence on optimal treatments for this condition. There is a need for high quality, randomized, and placebo-controlled research to establish the effectiveness of treatments in the management of De Quervain’s tenosynovitis. Although corticosteroid injection and surgery show some favourable outcomes, the qualities of evidence are low and adverse effects are evident. At present, it is reasonable to consider splinting as the most appropriate palliative treatment for De Quervain’s tenosynovitis because it is inexpensive, simple, and less invasive.
Functional Aims and Goals
[edit | edit source]The aim of the orthotic device is to provide rest to the wrist and the thumb in a functional position to help reduce swelling and associated pain. A static splint such as a wrist-thumb spica splint (also known as a long opponens splint or long thumb spica splint) made from low temperature thermoplastic (LTT) is one of the recommended orthotic devices, which restrict movements of the thumb and wrist to enhance healing of the thumb APL and EPB tendons. The first functional goal of the splint is to immobilise the wrist to restrict wrist flexion, extension, ulna deviation and radial deviation. The second goal is to immobilise the thumb carpometacarpal (CMC) and metacarpophalangeal (MCP) joints to prevent thumb flexion, extension, adduction and abduction. Together, this provides support and protection to the thumb APL and EPB tendons during the healing process and reduces associated symptoms. Concurrently, the splint prevents further stress and friction to the APL and EPB tendons during repetitive daily activities, which could aggravate the injury. The splint typically stabilises the wrist in 10-20˚ of extension and positions the thumb in 40˚ of CMC abduction and 10˚ MCP flexion (Hart et al., 2005). This enables thumb opposition to the index and middle fingers, which keeps the hand in a more functional position. Additionally, the interphalangeal (IP) joint of the thumb as well as the MCP and IP joints of the other fingers are free to move to allow the use of the hand for light activities.
A plaster of paris (POP) cast could also be used for long-term immobilisation of the wrist and thumb, in positioned as described above. However, the cast is a circumferential immobiliser that is inflexible and not removable, which can cause problems in patients with De Quervain’s tenosynovitis due to tissue swelling. A LTT splint, on the other hand, is a semi-circumferential immobiliser that is removable and adjustable with straps, which can accommodate swelling without becoming too tight. Moreover, management for De Quervain's tenosynovitis is ideally short-term, therefore a splint will be recommended over a POP cast.
Design
[edit | edit source]Materials
[edit | edit source]A volar-based wrist-thumb orthosis was made from a low temperature thermoplastic (LTT) material, which is malleable at low temperature (60˚-80˚). It is lightweight, easy to use, neat and heat-adjustable, which makes it easy to mold and contour directly on the patient’s hand.
Trimlines
[edit | edit source]
- The LTT wrist-thumb orthosis covers the volar aspect of the wrist and the arm. The volar side is able to tolerate more pressure than the dorsal side because it thicker with more subcutaneous tissue to disperse forces.
- The width of the device is 1/2 the circumference of the forearm. A larger surface area decreases more pressure (Jacobs & Austin, 2003, p.60-62).
- The length of the device extends from 2/3 the length of the forearm to palmar crease and thumb IP joint. This allows for a long lever arm, which adequately distributes pressure over the arm. However, elbow also needs to fully flex without interference and skin irritation (Jacobs & Austin, 2003, p.60-62).
- The proximal edges of the device is flared to ensure comfort and prevent skin irritation.
- The palmar crease edges and the thumb IP joint edges are folded to ensure comfort and prevent skin irritation.
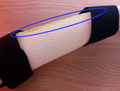
Strapping
[edit | edit source]- Three velcro straps (over the dorsal aspect of the arm, wrist and hand) are used to secure the device firmly to the arm as well as apply a three-point force system to maintain position. The straps are attached at the distal end of the device, over the wrist and the proximal end of the device.
- Wider straps are preferred because it prevents excess movement and friction, distribute the compressive force over a greater surface area and help reduce pressure (Jacobs & Austin, 2003, p.67).
Positioning
[edit | edit source]Correct positioning of the device onto the hand is critical, improper device can worsen injuries and even lead to deformities and complications. The wrist-thumb orthosis usually rest the wrist and the thumb joints in the following positions (Hart et al., 2005):
- Wrist: 10-20˚ extension, neutral wrist deviation
- Thumb CMC joint: 40˚ palmar abduction
- Thumb MCP joint: 10˚ flexion
- All other joints: did not immobilize, free for full range of motion.
Force Diagram
[edit | edit source]

Wrist-thumb orthosis are first-class levers (Duncan, 1989). There are two three-point force systems applied to maintain wrist extension and thumb abduction/extension position.
- Force 1 (F1): occurs at the wrist joint, which acts as the axis or the fulcrum.
- Force 2 (F2): occurs at the forearm (proximal end of the device), which serves as the force arm
- Force 3 (F3): occurs at the palmar aspect of the hand (distal end of the device), which acts as the resistance arm to the weight of the hand.
Orthosis should cover the three points of pressure force comfortably. The proximal (F2) and distal (F3) ends of the device act as the counterforce against the opposing middle force supplied by the dorsally placed wrist strap (F1).
- Force 4 (F4): occurs at the CMC joint
- Force 5 (F5): occurs at the MCP joint
- Force 6 (F6): occurs at the IP joint
The device covers the thumb up to the proximal IP joint to maintain thumb position.
Manufacturing process
[edit | edit source]Pattern
[edit | edit source]- Trace around hand (thumb extended and digits adducted) and 2/3 length of the forearm on a piece of paper
- Mark distal palmar crease, wrist joint and thumb CMC, MCP and IP joint
- Join the marks for palmar crease and thumb IP joint
- Add a tab between the thumb and the index finger and a tab between the thumb IP and MCP joint
- Draw pattern 2-3cm wider than the hand and the forearm
- Cut out the pattern and place it onto the patient's hand to check for correct fit and position
- Transfer pattern onto the LTT and then cut out using shears
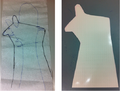
-
Pattern on Paper & LTT
Position the Patient
[edit | edit source]- Elbow supported, forearm vertical in neutral rotation
- Position the wrist and thumb joints into the required angles as described under ‘Design: Positioning’
-
Arm & Hand Positioning
Application
[edit | edit source]- Warm up LTT in a water bath at low temperature (60˚-70˚)
- When LTT is soft, remove and roll the palmar crease edges away from the skin
- Rewarm LTT. When LTT is soft, remove and place LTT onto the patient's hand and forearm
- Align LTT on the distal palmar crease and in the centre of the forearm
- Secure LTT by joining the tabs at the thumb and wrapping the medial and lateral sides around the forearm
- Mold LTT to contour the hand and forearm, whilst maintaing the correct position at all time.
- Smooth the LTT to avoid air pockets
- Mark medial, lateral and proximal trimlines
- Cut excess material at the trimlines
- When LTT returns to its rigid form, remove the LTT from the hand/forearm
Finishing Off
[edit | edit source]- Rewarm the proximal edge of the device and flare slightly
- Rewarm the distal edge of the thumb and roll the edge to below the IP joint
- Round and smooth the trimlines to ensure the trimlines are not uncomfortable or shape
-
Flaring & Rolling Thumb Edge
Strap Attachment
[edit | edit source]- Cut out loop Velcro to appropriate size and permanently attach to the lateral side of the thumb (by using a heat-gun to heat the LTT and the Velcro to ensure a strong bond). Attach self-adhesive hook Velcro to the medial side of hand
- Attach one self-adhesive hook Velcro to the volar surface of the device at the wrist joint. Use loop Velcro as a strap.
- Attach two self-adhesive hook Velcro to the volar surface of the device at the proximal edge of the device (making a V shape to allow loop Velcro strap to contours the arm). Use loop Velcro as a strap.
- Fit the device onto the patient's hand/arm and examine the function of the device.
-
Final Orthosis and Straps
-
Views of the Orthosis- Volar, Dorsal, Lateral and Medial
Critique of fit
[edit | edit source]The Client
- The client is a 35-year-old female, who is presented with sharp pain and swelling over the radial side of her right wrist and near the base of the thumb.
- The client reported that the pain has been present for three weeks and was worst when lifting and carrying her infant. She has also taken time off from work because the pain makes it difficult for her to play the piano.
Objective Assessment
A physical assessment was completed and revealed the following:
- Palpating over the radial side of the wrist and the thumb: Swelling at the radial styloid
- Active, resisted and passive wrist and thumb ROM tests: Decreased thumb ROMs, and pain sensation around the thumb and the wrist
- Finkelstein’s test (diagnosis test for De Quervain’s Tenosynovitis): Positive for pain over the radial styloid
-
Finkelstein's Test
Diagnosis
From the clinical assessment, the client is likely diagnosed with De Quervain’s Tenosynovitis, a painful wrist condition caused by an inflammation of the thumb tendons, abductor pollicus longus (APL) and extensor pollicis brevis (EPB), from overuse and repetitive wrist-thumb movements (Kay, N. R. 2000; Ranney, Wells, & Moore, 1995).
Prescription and Goals
- The client’s goals are to have no pain when lifting her child, and to return to playing and teaching the piano as soon as possible.
- In order to achieve these goals, the client was prescribed to wear a custom-made LTT wrist-thumb orthosis for 4 weeks. The aim of the orthosis is to immobilise the wrist and the thumb, thereby allowing the thumb tendons to heal, reducing pain and swelling as well as protecting the wrist and thumb from daily activities that could aggravate symptoms. The orthosis holds the wrist in 10-20˚extension and the thumb in 40˚ palmar abduction and 10˚ flexion. While the thumb IP joint and digit two to five are left free to move (Hart et al., 2005). This maintains the hand in a functional position, to use for daily light activities.
Device Presentation and Fitting
- The device fitted well on the client with good skin contact. It contoured the hand and arm nicely. Surface was neat and smooth, no noticed pressure points around bony prominence.
-
Volar & Dorsal Views of Orthosis
- The device achieved the goal to immobilised the wrist and the thumb CMC and MCP joint, while allowing the thumb IP joint and digit 2 to 5 to move freely.
- The device also achieved to hold the thumb and wrist in appropriate angles (thumb in slight abduction and flexion, and wrist in slight extension) to allow for some ROM for hand function. The client was able to do the following:
-
Opposed thumb to 2nd, 3rd and 4th finger
-
Fist
-
Open hand & Closed hand
Straps
- The straps are positioned appropriately, applying a three-point force system to maintain the required wrist position.
-
Three-point force system
- However, the straps can pinch and rub on the skin, which could cause chafing on the dorsal surface of the arm and hand. To address this issue, I could add foam padding on the straps.
-
Straps pinching/rubbing against the skin
Trimlines
- The distal trimline was rolled over away from the hand proximal to the palmar crease to allow for comfort and hand function, as described above. However, the trimline at the thumb was distal to the IP joint and the thumb circumference was small, thus limiting thumb flexion and causing discomfort and redness. To address this, I could reheat the area and roll the edges further down so that it is proximal to the IP joint and to widen the plastic out.
-
Limited IP joint flexion
- The proximal trimline was 2/3 the length of the forearm. This allows a long lever arm to reduce the required force to immobilise the wrist. The proximal edge was flared to prevent excessive pressure along the edge. Also, the proximal trimline was appropriate not to interfere with elbow movements:
-
Elbow Extension
-
Elbow Flexion
- Medial and lateral trimlines extended to approximately more than 1/2 the circumference of the forearm. This reduces the pressure on the arm due to the large surface area. The edges are neat and smooth to avoid creating pressure points, irritation, redness and discomfort.
-
Medial & Lateral Trimlines
- There were also visible trimline markings on the device because I cut below the markings- to address this issue, I should cut above the markings.
-
Trimline Marking
Alternative Design
An alternative design could be a LTT radial-based thumb orthosis that still immobilises the wrist and thumb, however, the orthosis fits on the radial half of the hand and arm, while leaving the ulnar border of the hand free for more functional use.
Justification of the Device with Outcome Measures
To evaluate the client's disability and pain status, and measure the effect of the orthosis, "The Dash: Disabilities of the Arm, Shoulder and Hand Outcome Measure" questionnaire was completed prior to treatment, mid-treatment (2 weeks later) and post-treatment (5 weeks later) and the client scored the following:
- Disability/symptom score (prior to treatment): 67.5/100
- Disability/symptom score (mid-treatment): 55.8/100
- Disability/symptom score (post-treatment): 18.3/100
A lower score indicates lesser disability and symptom, and a 10-point differences in scores can be considered an important change (Gummerson, Atroshi & Ekdahl, 2003).
With the orthosis on, the client scored 55.8%, showing an improvement in wrist and hand pain but no change in functionality. This demonstrated that the orthosis had achieved the aim of reducing pain and preventing the client from performing activities that may aggravate the injuries. Subsequently, the client scored 18.3% post-treatment, showing improvement in both pain and functionality, which indicates that the orthosis did provide some functional benefits.
Outcome measures
[edit | edit source]Traditionally, evaluating wrist and hand function following an intervention consist of measuring range of motion, strength and sensation. Nowadays, outcome measures are required to take into account patient’s ability to carry out activities of daily living and the ability to return to work (MacDermid et al., 2002). These subjective measures that assess the ability to function in daily life ensures that the treatment and evaluations focus on the patient rather than on the disease (Higginson & Carr, 2001; MacDermid et al., 2002).
The DASH (Disabilities of the Arm, Shoulder and Hand) questionnaire was used to determine my client’s disability and pain status as well as evaluate the functional benefits of the orthosis prescribed. The DASH is a 30-item questionnaire that assesses both symptoms and physical function with a five-response option for each item. The DASH contains questions of importance to the patient: pain, aspects of activities of daily living (ADL), confidence and participation in work and other social activities.
The DASH was selected for my client with De Quervain’s tenosynovitis because it is the most widely tested instrument for patients with wrist and hand injuries (Hoang-Kim, Pegreffi, Moroni, & Ladd, 2011). Systemic reviews have demonstrated that the DASH has good construct validity, test-retest reliability and responsiveness, making it an ideal outcome measure (Changulani, Okonkwo, Keswani, & Kalairajah, 2008). Additionally, The questionnaire is easy to administer, score and interpret data.
The client was asked to complete The DASH questionnaire prior to treatment, during-treatment (2 weeks later) and post-treatment (5 weeks later) and the client scored the following:
Prior to treatment: Disability/symptom score= 67.5/100
- The higher the score, the greater the disability and pain the client is in. 67.5% indicated the client was in great pain and had great disability to perform certain activities, especially activities that require the hand to twist, grasp and lift items. This coincides with the symptoms for De Quervain's tenosynovitis.
-
The Dash Results: Prior to treatment
During-treatment: Disability/symptom score= 55.8/100
- Two weeks with the orthosis on, the client had reduced pain (indicated in question 24-29), however, physical function and performing activities were limited. This was expected, because the orthosis was designed to allow hand function for only light activities. The orthosis successfully achieved the aim of preventing repetitive and overuse of the hand, to allow the thumb tendons to heal and avoid further injury.
-
The Dash Results: During-treatment
-
Outcome Measures: Opening a tight jar
-
Writing
-
Turning a key
Post-treatment: Disability/symptom score= 18.3/100
- One week after the orthosis was removed, there was a significant reduction in pain and an improvement in the ability to perform activities of daily living. Confidence and participation in work and other social activities was also scored better. There is a 49.2-score difference between post-treatment and prior to treatment. Gummesson et al. (2003) showed that a 10-point difference in DASH score can be considered as an important change. Overall, this suggests that the orthosis provided symptom and functional benefits to the client with De Quervain’s tenosynovitis.
-
The Dash Results: Post-treatment
Referral Letter to Physiotherapy
[edit | edit source]Reference
[edit | edit source]Alemohammad, A. M., Yazaki, N., Morris, R. P., Buford, W. L., & Viegas, S. F. (2009). Thumb interphalangeal joint extension by the extensor pollicis brevis: association with a subcompartment and de Quervain's disease. J Hand Surg Am, 34(4), 719-723. doi: 10.1016/j.jhsa.2008.12.015.
Ashurst, J. V., Turco, D. A., & Lieb, B. E. (2010). Tenosynovitis caused by texting: an emerging disease. J Am Osteopath Assoc, 110(5), 294-296.
Cardone, D. A., & Tallia, A. F. (2002). Joint and soft tissue injection. Am Fam Physician, 66(2), 283-288.
Clarke, M. T., Lyall, H. A., Grant, J. W., & Matthewson, M. H. (1998). The histopathology of de Quervain's disease. J Hand Surg Br, 23(6), 732-734.
Changulani, M., Okonkwo, U., Keswani, T., & Kalairajah, Y. (2008). Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop, 32(1), 1-6. doi: 10.1007/s00264-007-0368-z.
Dawson, C., & Mudgal, C. S. (2010). Staged description of the Finkelstein test. J Hand Surg Am, 35(9), 1513-1515. doi: 10.1016/j.jhsa.2010.05.022.
Duncan, R. M. (1989). Basic principles of splinting the hand. Phys Ther, 69(12), 1104-1116.
Gummesson C., Atroshi I. & Ekdahl C. (2003). The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord, 4(1), 11 doi:10.1186/1471-2474-4-11.
Hart, R. G., Kleinert, H. E., & Lyons, K. (2005). A modified thumb spica splint for thumb injuries in the ED. Am J Emerg Med, 23(6), 777-781. doi: 10.1016/j.ajem.2005.03.004.
Harvey, F. J., Harvey, P. M., & Horsley, M. W. (1990). De Quervain's disease: surgical or nonsurgical treatment. J Hand Surg Am, 15(1), 83-87.
Higginson, I. J., & Carr, A. J. (2001). Measuring quality of life: Using quality of life measures in the clinical setting. BMJ, 322(7297), 1297-1300.
Hoang-Kim, A., Pegreffi, F., Moroni, A., & Ladd, A. (2011). Measuring wrist and hand function: common scales and checklists. Injury, 42(3), 253-258. doi: 10.1016/j.injury.2010.11.050.
Howell, E. R. (2012). Conservative care of De Quervain's tenosynovitis/ tendinopathy in a warehouse worker and recreational cyclist: a case report. J Can Chiropr Assoc, 56(2), 121-127.
Huang, T. H., Feng, C. K., Gung, Y. W., Tsai, M. W., Chen, C. S., & Liu, C. L. (2006). Optimization design of thumbspica splint using finite element method. Med Biol Eng Comput, 44(12), 1105-1111. doi: 10.1007/s11517-006-0131-4.
Ilyas, A. M., Ast, M., Schaffer, A. A., & Thoder, J. (2007). De quervain tenosynovitis of the wrist. J Am Acad Orthop Surg, 15(12), 757-764.
Jacobs, M.L., & Austin, N. (2003). Splinting the Hand and Upper Extremity: Principles and Process. Baltimore, Md: Lippincott Williams & Wilkins.
Jongprasitkula, H., Suputtitadaa, A., Kitisomprayoonkula, W., & Pintawirujb, K. (2011). Elastic bandage vs. neoprene thumb stabilizer splint in acute De Quervain’s tenosynovitis. Asian Biomedicine, 5(2), 263-267. doi: 10.5372/1905-7415.0502.035.
Kay, N. R. (2000). De Quervain's disease. Changing pathology or changing perception? J Hand Surg Br, 25(1), 65-69. doi: 10.1054/jhsb.1999.0277.
Lane, L. B., Boretz, R. S., & Stuchin, S. A. (2001). Treatment of de Quervain's disease:role of conservative management. J Hand Surg Br, 26(3), 258-260. doi: 10.1054/jhsb.2001.0568.
MacDermid, J. C., Fess, E. E., Bell-Krotoski, J., Cannon, N. M., Evans, R. B., Walsh, W., . . . Santore, G. (2002). A research agenda for hand therapy. J Hand Ther, 15(1), 3-15.
Moore, J. S. (1997). De Quervain's tenosynovitis. Stenosing tenosynovitis of the first dorsal compartment. J Occup Environ Med, 39(10), 990-1002.
Muckart, R. D. (1964). Stenosing tendovaginitis of abductor pollicis longus and extensor pollicis brevis at the radial styloid (de Quervain's disease). Clin Orthop Relat Res, 33, 201-208.
Neumann, D. A., & Bielefeld, T. (2003). The carpometacarpal joint of the thumb: stability, deformity, and therapeutic intervention. J Orthop Sports Phys Ther, 33(7), 386-399. doi: 10.2519/jospt.2003.33.7.386.
Ranney, D., Wells, R., & Moore, A. (1995). Upper limb musculoskeletal disorders in highly repetitive industries: precise anatomical physical findings. Ergonomics, 38(7), 1408-1423. doi: 10.1080/00140139508925198.
Read, H. S., Hooper, G., & Davie, R. (2000). Histological appearances in post-partum de Quervain's disease. J Hand Surg Br, 25(1), 70-72. doi: 10.1054/jhsb.1999.0308.
Richie, C. A., 3rd, & Briner, W. W., Jr. (2003). Corticosteroid injection for treatment of de Quervain's tenosynovitis: a pooled quantitative literature evaluation. J Am Board Fam Pract, 16(2), 102-106.
Sakai, N. (2002). Hand pain attributed to overuse among professional pianists: a study of 200 cases. Medical Problems of Performing Artists, 17(4), 178-180.
Sampson, S. P., Wisch, D., & Badalamente, M. A. (1994). Complications of conservative and surgical treatment of de Quervain's disease and trigger fingers. Hand Clin, 10(1), 73-82.
Ta, K. T., Eidelman, D., & Thomson, J. G. (1999). Patient satisfaction and outcomes of surgery for de Quervain's tenosynovitis. J Hand Surg Am, 24(5), 1071-1077. doi: 10.1053/jhsu.1999.1071.
Weiss, A. P., Akelman, E., & Tabatabai, M. (1994). Treatment of de Quervain's disease. J Hand Surg Am, 19(4), 595-598. doi: 10.1016/0363-5023(94)90262-3.
Wolf, J. M., Sturdivant, R. X., & Owens, B. D. (2009). Incidence of de Quervain's tenosynovitis in a young, active population. J Hand Surg Am, 34(1), 112-115. doi: 10.1016/j.jhsa.2008.08.020
Yassi, A. (1997). Repetitive strain injuries. Lancet, 349(9056), 943-947. doi: 10.1016/S0140-6736(96)07221-2.
Appendix 1: Search Strategy
[edit | edit source]Databases Searched: Pubmed, Medline, Cochrane Library
Search Terms:
- de Quervain’s tenosynovitis OR de Quervain’s disease
- Repetitive strain injury
- Abductor pollicis longus OR Extensor pollicis brevis
- Thumb spica OR thumb splint OR hand-wrist orthoses
- Treatments
Other:
Other papers were located by the reference lists of studies already obtained