Motivation and emotion/Book/2021/Lived experience in mental health professionals
What is the role of lived experience for mental health professionals?
Overview
[edit | edit source]|
True story: Juli received treatment for depression during her undergraduate degree in psychology. She had been practicing as a registered psychologist for several years when she experienced her first manic episode which lasted for 3 months. She was ill and did not realise it. As a dedicated psychologist, she experienced acute mental health needs, yet was apprehensive to disclose her experiences or seek help due to concerns about the professional risk to do so. With support from close colleagues, Juli eventually sought treatment. "Disclosure has not stopped me from working for a large health care system, being an Assistant Professor and Director of Clinical Training, and serving as the board president of a non-profit focused on suicide prevention ... (disclosure) was and continues to be the most powerful and courageous thing I have done in the field ..." - Juli (Vierthaler & Elliott, 2020, p. 2).
|

Mental health care intervention has progressed and changed a lot over the last 40 years, although understanding mental health, disorders, and effective treatment continues to evolve (Drake et al., 2003). The voices of those with lived experience of mental health problems have been, and continue to be, influential to this process particularly regarding advocacy efforts for rights-based changes to the mental health system (Probert, 2021).
Current evidence suggests that mental health professionals are not immune to mental health difficulties or mental illness (Elliott & Ragsdale, 2020) and many professionals have reported seeking psychotherapy at some point (Victor et al., 2021) (Figure 1). This chapter explores the growing research of lived experience from a mental health professional perspective (King et al., 2020), and the associated benefits and challenges that lived experience have for mental health professionals.
|
Focus questions:
|
Definitions
[edit | edit source]
Mental health and mental illness
[edit | edit source]Mental health is a state of emotional, psychological, and social well-being (Westerhof & Keyes, 2010) whereby an individual realises:
- their abilities
- they can cope with the normal stresses of life
- they can work productively
- they can contribute to their community.
Mental health is said to be central to functioning and life enjoyment as individuals and as a society (Gilmour, 2014).
Mental health and mental illness are related yet separate aspects of psychological well-being (Westerhof & Keyes, 2010). The concept of mental illness, like physical illness, encompasses a broad range of conditions such as brain diseases and disorders which explain mental and behavioural disturbances, bound by the jurisdiction of psychiatry (Insel & Wang, 2010) (Figure 2).
Lived experience
[edit | edit source]There is a lack of consensus in defining 'Lived experience' although previous literature has focused on individual experiences relating to diagnosis, service-use, and life-changing effects of mental health challenges (Roenndfeldt & Byrne, 2020). Lived experience is based on a belief that consumers are 'the experts' of their own lives and carry the wisdom to best articulate their needs.
|
A closer look at lived experience (YouTube)
|
History of mental health treatment
[edit | edit source]
Historically, mental health was conceptualised differently. It was assumed that people with mental illness:
- had no capacity to look after themselves
- should be separated from the rest of society
- were people considered ‘dangerous’
- should live in gaol or asylums (Figure 3)
- some were considered 'insane' and seen to be responsible for their illness due to moral weakness and personal deficiency.
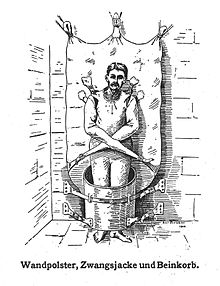
Personal rights aside, patients were often subject to treatments (Figure 4) including heavy sedation, electroconvulsive therapy and lobotomy (Figure 5) which was commonly performed in the 1900s to calm and control violent or emotional patients. Results of lobotomies (Figure 7) ranged from poor impulse control, absence of feeling, patients that were unnaturally calm and shallow, and even death. After subjecting tens of thousands of people to this procedure worldwide, eventually, this was replaced with the introduction of psychoactive drugs (Foerschner, 2010). With the introduction of medications to control symptoms, eventually, there was a human rights movement to deinstitutionalise people however, this led to other problems including high rates of homelessness and incarceration (Foerschner, 2010).



|
More on history (YouTube)
BBC Mental - A History of the Madhouse - full documentary |
|
Focus questions:
|
How has lived experience shaped mental health care?
[edit | edit source]
Mental health has an alarming history. It has been the voices of those with lived experience of mental health difficulties that have significantly influenced thoughts, beliefs, and approaches to mental health care (Figure 8) which has helped shape the following:
Mental health service design, delivery, and evaluation
[edit | edit source]Those with lived experience have been actively, and more increasingly, involved in the design, delivery, and evaluation of mental health services (Nilsen et al., 2013 cited in Scholz et al., 2017).
Examples of changes include:
- balance of power shifted to place mental health service users on an equal footing with professionals
- it was recognised that mental health consumers have expertise in their knowledge of mental illness
- health policy began to support the active participation of consumers, families, and carers in all aspects of policy, planning, and services.
Policy indicates involvement is now required from those with lived experiences at all levels of the mental health system (Scholz et al., 2017). For example:
- individual level (i.e., in one’s own health care plan)
- the organisational/service level (i.e., in roles for shaping services etc)
- the system level (i.e., for broader roles such as in shaping policy).
Recovery approaches
[edit | edit source]
With the consumer movement and recognition of lived experience, Recovery approaches were developed as an alternative way of thinking compared to the medical model which has an emphasis on pathology, deficits, and dependency (Figure 9). Muir-Cochrane et al., (2018), define recovery as a personal journey where meaning and purpose are central to a person's life despite diagnosis. Central to all recovery paradigms is hope, self-determination, self-management, empowerment, and advocacy. Also key is a person's right to full inclusion and meaningful life of their own choosing, free of stigma, and discrimination.
Some characteristics of recovery commonly cited are that it is:
- a unique and personal journey
- a normal human process
- an ongoing experience and not the same as an endpoint or cure
- a journey rarely taken alone
- nonlinear—frequently interspersed with both achievement and setbacks (Jacobson and Greenley, 2001).
|
More on recovery (YouTube)
|
Workforce
[edit | edit source]Lived experience has increasingly emerged as being a desirable, sought-after quality in the workforce as an alternative to the traditional mental health worker role and is even considered best practice. Workers with lived experience have specialised knowledge and skills of mental health challenges, service engagement, and recovery, unique in supporting mental health consumers. Evidence indicates that workers with lived experience are just as effective at supporting consumers as traditional mental health workers (Roennfeldt & Byrne, 2020). However, there are still challenges for those with lived experience in these settings. For example, findings suggest that organisational health settings need to create cultural norms that are more inclusive and empowering of those with lived experience (Scholz et al., 2020).
Education
[edit | edit source]It is suggested that those with lived experience are in the best position to genuinely understand, explain, and convey stories of the very internal, individual, and unique processes of recovery that cannot be seen or understood from an observer. Further, it is indicated that those who have struggled then overcome mental distress are in an ideal position to teach others about these issues including challenging mental health professionals who hold stigmatising views and increasing consumer participation (Byrne et al., 2012).
For example, research findings suggest that student nurses were positively influenced by recovery concepts taught by an academic who had lived experience of significant mental health challenges, and recommendations were made to utilise educators with lived experience as an educational strategy (Byrne et al., 2012). However, Practice Guidelines are useful for those intending to co-produce learning programs.
Recovery Colleges
[edit | edit source]
There has been emerging research into recovery colleges (Figure 10) whereby those with lived experience work with a mental health professional to deliver a structured course designed to improve participants' understanding of mental health, wellbeing, and recovery. Research into recovery colleges has thus far been positive and reinforces the value of lived experience knowledge base applied to an educational setting (Muir-Cochrane et al., 2019). Findings indicate the following outcomes for participants:
- improved wellness
- reduced feelings of isolation
- improved clinical and wellbeing indicators
- reduced mental health service use
- achievement of personal goals
- transforming attitudes of clinical staff and mental health services
- hope (for recovery and for the future)
- identity (realising new possibilities related to self e.g. patient to student)
- recovery colleges are described as transition spaces (through experience and outcomes) (Muir-Cochrane et al., 2019).
“ I'm a different person...I've reclaimed my life...recovery college is one of the most powerful things that happened to me in my life ” — Recovery College Participant (Muir-Cochrane et al., 2019, p.4)
|
More about Recovery Colleges (YouTube)
|
Research
[edit | edit source]- Psychological science has developed value in the lived experiences of people as an area of expertise and knowledge especially given reform in mental health care over the last three decades (Picton et al., 2017).
- Phenomenology is a methodology that is applicable for psychological research involving people with mental illness and guides researchers in the field of lived experience (Picton et al., 2017). Phenomology is the study of human experience and mental processes, and the meaning, knowledge, and insight that is derived from lived experiences which are considered subjective and interpretive (Denscombe, 2010).
|
True story: Dr Elyn Saks is Associate Dean and Professor of Law, Psychology, and Psychiatry and the Behavioral Sciences at the University of Southern California Gould Law School, and an expert in mental health law. Saks lives with schizophrenia and has written about her experience with the illness starting from age 8 in her autobiography. She has a PhD in psychoanalytic science and has contributed valuable research within the mental health field including exploring excessive use of force in encounters between law enforcement and individuals with mental health challenges. |
Lived experience and mental health professionals
[edit | edit source]Mental health professionals are not immune to mental health difficulties (Elliott & Ragsdale, 2020). An increasing number of high-functioning, successful mental health professionals have/continue to publicly disclose their struggles (Vierthaler & Elliott, 2020). The following explores the types of mental health professional titles, disclosures of personal mental health struggles in the field, and the challenges and benefits of having lived experience whilst working in this field.
Types of mental health professionals
[edit | edit source]
There are mental health professionals who have a lived experience of mental illness and they are referred to as "prosumers" (Boyd et al, 2016) (Figure 11). There are many types of health professionals who work in mental health care including:
- your doctor
- counsellors
- psychiatrists
- psychologists
- occupational therapists
- mental health nurses
- community health workers
- social workers
- peer support workers
Types of mental health challenges for mental health professionals
[edit | edit source]Several journal articles explore the lived experience of mental health distress in mental health professionals. Sharing personal journeys of lived experience publicly aims to promote understanding, empathy, hope for recovery as well as fight stigma and discrimination amongst prosumers (Vierthaler & Elliott, 2020). Examples include:
- Psychologist - depression with mania and psychosis (Vierthaler & Elliott, 2020).
- Psychiatrist - bipolar disorder with attacks of mania, depression, and psychosis (Freisen, 2020).
- Psychologists - non-suicidal self-injury (Victor et al., 2021).
- Psychologists - burnout, distress and negative affect can result from work with clients (Scibberras & Pilkington, 2018).
|
More about lived experience for mental health professionals (YouTube)
|
Psychological Theory
[edit | edit source]
Childhood trauma
[edit | edit source]Research into the backgrounds of mental health professionals suggests that many were raised in dysfunctional, traumatic family environments in childhood and often experience psychological distress later in life (Elliott & Guy, 1993). One study found that psychotherapists experienced higher incidences of physical abuse, sexual abuse, parental alcoholism, psychiatric hospitalisation of a parent, death of a family member, and greater dysfunctional families than those in non-mental health professions (Elliott & Guy, 1993).
Wounded Healer Paradigm
[edit | edit source]The Wounded Healer is based on the idea that childhood experiences of dysfunction and trauma are the primary motivators for working in the psychology field and that those in healing roles choose their profession based on their history of pain, suffering and confronting adversity (Figure 12). It is said that this woundedness is drawn on to assist with others healing such as deep empathy to facilitate connection. However, it is understood that those who do not tune in to their vulnerabilities and difficulties impair the healing role; there is a difference between a Wounded Healer and an impaired professional. The Wounded Healer construct is not new and stems back to Greek mythology over 2,500 years ago. Jung was quoted as saying 'only the wounded physician heals', in the 1960s (Zerubavel & O'Dougherty Wright, 2012).
Barriers and challenges
[edit | edit source]Research indicates that mental health professionals with lived experience can be impacted by the following themes.
Identity
[edit | edit source]Mental health professionals with lived experience have expressed a state of disharmony, or conflict concerning their identities as both professional and service-user further affecting the combining of their clinical and experiential knowledge, a common theme identified when synthesizing 23 studies; 'negotiating hybrid identities' (King et al., 2020). Many mental health professionals can feel pressure to appear invulnerable and to remain firmly on the side of the ‘helper’ (Figure 13) (Kemp et al., 2020).
Culture of non-disclosure
[edit | edit source]A culture of non-disclosure exists for mental health professionals in workplaces contributing to stigmatising attitudes and behaviour (King et al., 2020). While some professionals are open about their lived experience of mental health difficulties and consider this as advantageous, others indicate caution about disclosure. Boyd et al. (2016), indicated that two-thirds of respondents in their research did not disclose to their patients and only a small few of those respondents disclosed to colleagues. Byrne et al. (2012) discussed a need for attitudinal change.
Stigma
[edit | edit source]Studies indicate that mental health professionals with mental illness face stigma similar to, or even worse than stigma towards non-professionals in the general population (Elliott & Ragsdale, 2020). Multiple studies indicate that internalising stigma is evident within the field (Boyd et al., 2016). King et al., (2020) identified stigmatising themes through synthesising 23 independent studies and these are said to influence sharing lived experience in the workplace, including, 'impaired professional' and 'the “us and them” divide'.
“ ...stigma is still prevalent even in organisations that have consumers in leadership positions, and consumers are often perceived as less able to work in mental health organisations than non-consumers (Scholz et al., 2018, p.1). ”
Counter-transference
[edit | edit source]There is a need to recognise counter-transference responses and internal conflicts of the therapist (Wheeler, 2007) and it has been suggested that empathy work can trigger own symptoms (Elliott & Ragsdale, 2020).
Benefits
[edit | edit source]Research indicates that mental health professionals with lived experience can be valuable in the following ways:

Reducing Stigma
[edit | edit source]- High functioning professionals are in a valuable position to decrease stigma (Figure 14), discrimination and increase individuals' concepts of hope for recovery (Boyd et al., 2016).
- Mental health professionals with a diagnosis can contribute to the mental health field by countering stigma, strengthening the recovery movement and being visible as a prosumer to model wellness. (Vierthaler & Elliott, 2020).
- The British Psychological Society has recommended a revision of the way mental distress is considered given a plethora of evidence that it is on a 'spectrum with normal experience' and that there can be standard causal psychological factors such as employment, poverty, and trauma (Propert, 2021).
- Destigmatising themes identified through synthesising 23 studies include, 'the “wounded healer”' and 'belief in the continuum of emotional distress' (King et. al., 2020).
Lived experience as an asset
[edit | edit source]- Studies show that mental health professionals see their lived experience as an asset and also advocate for their self-care to continue in their professional work (Boyd et al., 2016).
- Studies are increasingly exploring lived experience and disclosure within the scope of the therapeutic relationship between health professionals and service users (King et al., 2020).
- The British Psychological Society (2020), released a formal statement acknowledging lived experience as an asset to the profession, indicated the significant contribution that can be made by those who have experienced mental health difficulties, and highlighted that lived experience does not need to be seen as a barrier to training or practicing as a psychologist.
- Those with lived experience bring value to mental health organisations given their expertise in the mental health system, and their ability to provide safety and support to other consumers - lived experience is like 'a sneaky, special degree' (Scholz et al., 2018).
- There are things you cannot learn from books (Byrne et al., 2012).
| “ | For those we treat to trust in us, we ourselves need to trust in what we promote. Individuals with mental health struggles can and do recover (American Psychological Association & Jansen, 2014, cited in Vierthaler & Elliott, 2020, p.3). | ” |
Have your say
[edit | edit source]What are your thoughts about seeking assistance from mental health professionals with lived experience - complete the quick, anonymous Poll (Figure 15). Poll results visible on completion.

Conclusion
[edit | edit source]- Lived experience has been vital to progression and changes in many areas of the mental health system especially for personal rights, increasing hope for recovery and reducing stigma.
- Mental health professionals experience mental health difficulties and mental illness just as the general population does, however, stigma may affect professionals worse than the general public if disclosed.
- Evidence suggests that many mental health professionals are motivated to enter the industry due to their prior struggles and experiences.
- Mental health professionals with lived experience can be helpful during the therapeutic process for those seeking treatment given the depth of personal and professional knowledge, however, lived experience can also hinder the process if professionals' difficulties or distress are not managed.
- It is suggested that the industry needs to progress towards being more open and support those with lived experience as well as provide recommendations to foster safety, resilience and post-traumatic growth (Zerubavel & Wright, 2012).
- Findings suggest that interventions to support professionals to share their lived experience may improve workplace diversity and well-being (King et al., 2020).
See also
[edit | edit source]- Vicarious trauma effects on the emotionality of mental health workers (Book chapter, 2016)
- Wounded healer paradigm (Book chapter, 2021)
References
[edit | edit source]British Psychological Society. (2020). Statement on clinical psychologists with lived experience of mental health difficulties. [online] Available at: <https://www.bps.org.uk/sites/www.bps.org.uk/files/Policy/Policy%20-%20Files/Statement%20on%20clinical%20psychologists%20with%20lived%20experience%20of%20mental%20health%20difficulties.pdf> [Accessed 21 October 2021].
Byrne, L., Happell, B., Welch, T., & Moxham, L. J. (2012). ‘Things you can't learn from books’: Teaching recovery from a lived experience perspective. "International journal of mental health nursing", 22(3), 195-204.
Denscombe, M. (2010). (4th ed). The good research guide for small scale social research projects. Maidenhead: Open University Pres McGraw Hill.
Drake, R., Green, A., Mueser, K., & Goldman, H. (2003). The history of community mental health treatment and rehabilitation for persons with severe mental illness. Community mental health journal, 39(5), 427-440.
Elliott, D., & Guy, J. (1993). Mental health professionals versus non-mental-health professionals: Childhood trauma and adult functioning. Professional Psychology: Research and Practic, 24(1), 83.
Elliott, M., & Ragsdale, J. (2020). Mental health professionals with mental illnesses: A qualitative interview study. American Journal of Orthopsychiatry, 90(6), 677–686. https://doi.org/10.1037/ort0000499
Foerschner, A. (2010). The History of Mental Illness: From" Skull Drills" to" Happy Pills". Inquiries Journal, 2(09).
Freisen, A. (2020, August 27). Changeover—How My Lived Experience Changed My Life, My Work as a Psychiatrist, and How It Resulted in the Establishment of a Support Group for Prosumers in Germany. Psychological Services. Advance online publication. http://dx.doi.org/10.1037/ser0000487
Gilmour, H. (2014). Positive mental health and mental illness. Statistics Canada.
Insel, T., & Wang, P. (2010). Rethinking mental illness. Jama, 303(19), 1970-1971.
Jacobson, N., & Greenley, D. (2001). What is recovery? A conceptual model and explication. Psychiatric services, 52(4), 482-485.
Kemp, N., Scior, K., Clements, H., & Mackenzie-White, K. (2020). Supporting and valuing lived experience of mental health difficulties in clinical psychology training. [ebook] British Psychological Society, pp.1-29. Available at: <https://www.bps.org.uk/sites/www.bps.org.uk/files/Member%20Networks/Divisions/DCP/Lived%20experience%20of%20mental%20health%20difficulties%20in%20clinical%20psychology%20training.pdf> [Accessed 21 October 2021].
King, A., Brophy, L., Fortune, T., & Byrne, L. (2020). Factors Affecting Mental Health Professionals’ Sharing of Their Lived Experience in the Workplace: A Scoping Review. Psychiatric Services, 71(10), 1047-1064. https://doi.org/10.1176/appi.ps.201900606
Muir‐Cochrane, E., Lawn, S., Coveney, J., Zabeen, S., Kortman, B., & Oster, C. (2019). Recovery college as a transition space in the journey towards recovery: an Australian qualitative study. Nursing & health sciences, 21(4), 523-530. https://doi.org/10.1111/nhs.12637
Picton, C., Moxham, L., & Patterson, C. F. (2017). The use of phenomenology in mental health nursing research.
Probert, J. (2021). Moving toward a human rights approach to mental health. Community mental health journal, 1-13.
Roennfeldt, H., & Byrne, L. (2020). How much ‘lived experience' is enough? Understanding mental health lived experience work from a management perspective. Australian Health Review, 44(6), 898-903. https://doi.org/10.1071/AH19261
Scholz, B., Bocking, J., & Happell, B. (2018). Improving exchange with consumers within mental health organisations: Recognising mental ill health experiences as a "sneaky, special degree". International Journal of Mental Health Nursing, 27(1), 227-235. doi:10.1111/inm.12312
Scholz, B., Stewart, S., Bocking, J., & Happell, B. (2017). Rhetoric of representation: The disempowerment and empowerment of consumer leaders. Health Promotion International, 34(1), 166-174. doi: 10.1093/heapro/dax070
Sciberras, A., & Pilkington, L. (2018). The lived experience of psychologists working in mental health services: An exhausting and exasperating journey. Professional Psychology: Research and Practice, 49(2), 151. https://doi.org/10.1037/pro0000184
Victor, S., Lewis, S., & Muehlenkamp, J. (2021). Psychologists with lived experience of non-suicidal self-injury: Priorities, obstacles, and recommendations for inclusion. Psychological services.
Vierthaler, J., & Elliott, E. (2020). A Shared Lived Experience of a Psychologist Battling a Mental Health Crisis. "Psychological Services". Advance online publication. http://dx.doi.org/10.1037/ser0000489
Westerhof, G., & Keyes, C. (2010). Mental illness and mental health: The two continua model across the lifespan. Journal of adult development, 17(2), 110-119.
Wheeler, S. (2007) What shall we do with the wounded healer? The supervisor's dilemma, Psychodynamic Practice, 13:3, 245-256, DOI: 10.1080/14753630701455838
Zerubavel, N., & Wright, M. O. D. (2012). The dilemma of the wounded healer. Psychotherapy, 49(4), 482.
External links
[edit | edit source]- A tale of mental illness from the inside Dr Elyn Saks and schizophrenia | TED(YouTube)
- Imagine There Was No Stigma to Mental Illness | Dr. Jeffrey Lieberman | TEDxCharlottesville (YouTube)
- in2gr8mentalhealth (Website)
- Mental health but not as you know it | Dr Louise Byrne | TEDxRockhampton (YouTube)
