Motivation and emotion/Book/2013/Pain and emotion
What is the role of emotion in the experience of pain?
Overview[edit | edit source] Pain and Emotion have a strong association with each other. When individuals experience feelings of emotional pain, the same areas of the brain is activated to when a person is affected by physical pain (Lumley et al., 2011). The fundamental basis of this chapter will underpin chronic pain as the main focus and analysing the relationship between emotions as it is facilitated through neurobiological, psychological, and social change. The International Association for the Study of Pain identifies pain as something that has an unpleasant sensory and emotional experience to a intense or harming stimuli(Lumley et al., 2011). Pain is hence at least a partial representation of an emotional experience. Often the response to pain is a negative feeling to withdraw or avoid further damage to the human body. The nervous system sends signals from sensory information gather by touch to avoid further tissue damage(Lumley et al., 2011). Similarly pain is an important part of experiencing the world, as it also provides associative learning to avoid certain danger. For example if an individual burns their hand on a hot frying pan, the burn is processed as unpleasant, and the next time they are near a hot frying pan they will avoid touching it.
|
Pain
[edit | edit source]Pain is most commonly experienced through a burn, laceration, or blunt force trauma to the human tissue, bone, or internal organs (Vogt, 2005). Pain is a strong motivator for individuals to withdraw from dangerous environments, by protecting a damaged area while it heals. Pain is an important response as it creates associative learning to avoid similar experiences in the future (Lumley et al., 2011). Common sensations involve feelings of burning, aching, freezing, nausea, stinging, and crunching to name a few. Often injuries such as laceration, burning, bites, fracturing, or blunt force trauma to the human tissue are the most common forms of injury (Vogt, 2005).

Types of Pain
[edit | edit source]Experts in medicine and psychology distinguish pain into two categories.Acute pain refers to the milder forms of pain which last for a relatively short period of time. Acute pain acts as an adaptive alarm to alert the individual of danger (Lumley et al., 2011). Chronic pain is a persistent and unpleasant experience which can last for an extended period of time - often at least 3 months (Lumley et al., 2011). Chronic pain is more problematic, as it can be quite debilitating in comparison. Pain also must go through a transitional period lasting only until the noxious stimulus is removed and has pathologically healed (Vogt, 2005). The experience of pain however is subjective to the individual, and although physicians have determined periods of time for pain to cross the threshold, a heuristic view is more suitable which identifies chronic pain existing when pain extends past the expected period of healing (Shyu & Vogt, 2009).

- Joint degeneration - osteoarthritis.
- Inflammation - inflammatory bowel disease.
- Tumor growth - cancer pain.
- Neuropathic pain - damaged nerves.
- Tissue anoxia - sickle cell disease.
- Occipital irritation - itchy eyes
- Arterial damage - heart attack, blood vessel damage.
Degree of Pain
[edit | edit source]Lumley and Colleagues (2011)identify several types of pain that are experienced based on symptoms. Visceral Pain involves pain in superficial structures. Deep somatic pain is caused by damage involving ligaments, tendons, bones, blood vessels, and muscle. This pain is considered aching, with poorly localization of pain. Superficial pain affects the upper dermal layer of skin or other superficial tissue, which causes a sharp and well-defined area of pain. Neuropathic pain is caused through damage or disease which effects the nervous system.
Classification
[edit | edit source]Pain is classified according to specific characteristics
- Region of body involved.
- Bodily System that is dysfunctional and may be causing the pain (nervous system, endocrine system, gastric system)
- Duration of pain
- intensity and time
- Epidemiology (the cause pain)
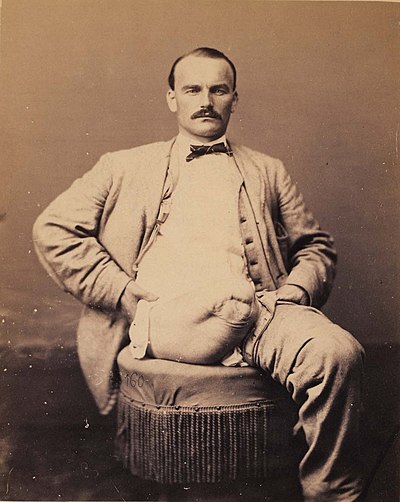
Phantom Pain
[edit | edit source]Phantom pain is a phenomenon that affects the neuropathic pain system. Phantom pain exists after the removal of a limb/organs which the brain no longer receives signals from (Prakash & Colwala, 2011). Phantom pain has a high prevalence effecting amputees. Some amputees describe the feeling of pain as shooting, crushing, burning or cramping. Some researchers suggest that if the pain is continuous for a long period of time, it may be assumed some parts of the intact body may become sensitized (Prakash & Colwala, 2011). The loss of sensations and voluntary motor control after serious spinal cord damage also shows signs of pain in places of complete sensory loss (Lumley et al., 2011).
Chronic Pain
[edit | edit source]Modern approaches to chronic pain suggests that when pain crosses the threshold of being acute, the adaptive alarm of acute pain will have lost some of it's efficiency as the pain no longer signifies damage to the tissue (Lumley et al., 2011). Similarly the behavioural change that is required to reduce pain may have become maladaptive. Primary and specialty pain clinics, as well as mental health and substance dependencies clinics treat chronic pain suffers on a regular basis. Pain is considered the most promonent issue faced by health care providers.
Somatoform/Social Pain
[edit | edit source]Somatoform or psychogenic pain, is a pain caused that is increased/prolonged by mental, emotional or behavioral factors. Often individuals stigmatize suffers of somatoform pain because they believe their pain is made up. However, somatoform pain stems from a psychological source and is just as detrimental to pain caused by other sources. Emotional pain due to social disappointments or frustrations, or emotional trauma resembles physical pain. Emotional hurt can emulate real physical pain, when you relieve hurt feelings (Lumley et al., 2011). Often individuals who have recently broken up with their partner experience real pain sourced from their heart. Experiences of rejections may lead to various physical pain disorders such as fibromyalgia (Kross, Berman, Mischel, Smith, & Wager, 2011). Similarly, social disappointment activates the same region of the brain assoicatied with the sensation of pain/ This is identified within thee Anterior Cingulate Cortex (Lumley et al., 2011). Social pain may be in part a form of somatization which appears to have a tendency to be experience and communicated disproportionate or excessive to pathological findings (Lumley et al., 2011).
Physiology of Pain
[edit | edit source]Nociception is a neural process of encoding and processing noxious signals through the afferent activity of the peripheral and central nervous systems (Ploner, Gross, Timmerman, & Schnitzler, 2006). Nociceptors better known as pain recepetors can detect mechanical, thermal or chemical change higher than the individuals threshold. Once stimulated a pain receptor transmits a signal along the spinal cord to the brain. According to Ploner and Collegues (2006) Pain sensation starts from a bare nerve ending and travels along The axons carrying pain information. Certain axon have little or no myelin sheath around it which therefore conducts impulses that are relatively slow between the range of 2 to 20 meters per second (m/s). This signal therefore is interpreted by the body as a slow dull pain. Similarly thicker and faster axons convey sharper pain such as a stabbing or cutting( Ploner et al., 2006). However, pain is interpreted fast and immediate in comparison to other sensations among the body. Pain sensation travels at a slower rate to the brain however the information is processed rapidly, this is due to the motor repossesses to pain are faster than motor responses to touch (Ploner et al., 2006). Pain axons release two neurotransmitters in the spinal cord. Mild pain produces the neurotransmitter glutamate, whereas stronger pain releases glutamate and substance P (Cao et al., 1998). Pain and touch spinal paths run parallel to each other, however the pain pathway crosses to the contralateral side of the spinal cord. Where as touch information does not cross until the medulla. Thus pain and touch reach at different sites in the cerebral cortex (Albanese, Duerden, Rainville, & Duncan, 2007). There is also a link that suggest that individuals that have a predisposition toward higher physical pain sensitivity have a biological vulnerabilitiy when the associated areas of the brain in or around the somatosensory cortex is activated (Kross, Berman, Mischel, Smith, & Wager, 2011).
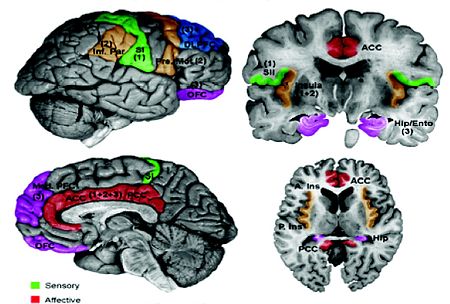
The Interaction of The Anterior Cingulate Cortex
[edit | edit source]Ringel and Collegues (2008) conducted a study on patients with irritable bowel syndrome, results provided that pain induces activity appear within the anterior cingulate cortex (aCC). Activation of the aCC is positively correlated with anxiety, stressful life events, and a history of abuse. The research suggests that the importance of early emotional experiences help facilitate pain response. Similarly treatment with psychological therapy has also shown to reduce pain and anxiety whilst reducing anxiety of the cingulate cortex (lackner et al., 2006). Hadjistavropoulos and Craig (2002) also conducted research on experiencing pain and observing individuals under painful injuries. Results showed activation in the aCC and the anterior insuls which showing empathic response that correlate with the intensity of pain.
Sensitization to Pain
[edit | edit source]Touching an already injured organ such as sunburn can send off signals to produce a pain reaction. Damaged tissue releases a chemical known as histamine and other chemicals which repair but also induce the response to nearby heat and pain receptors. Similarly, Substance P has been analyzed among rats . the result showed mice without Substance P can't detect increased intensity of pain (DeFelipe et al., 1998).Similarly Medial pain systems also spread to a number of subcortical sites that are key for emotions such as the amygdala, hypothalamus, and periaqueductal gray (Lumley et al., 2011). Pain induced sensitization of neurons within the Amydala of rats contributes to persistent pain affect that is associated with arthritis (Neugebauer, Galhardo, Maione, & Mackey, 2009). During this experiment, lesions or injecting morphine into the amygdala suppressed rats' emotional responses to a painful stimuli.
Emotional pain
[edit | edit source]Painful stimuli also activate a path that goes through the reticular formation of the medulla and then to several of the central nuclei of the thalamus, the amygdale, hippocampus, prefrontal cortex, and the cingulate cortex (Albanese, Duerden, Rainville, & Duncan, 2007). However these areas react to emotional associations. Such as watching someone you care about in pain. This is known as sympathetic pain (singer et al., 2004). Similarly Pain-sensitive cells in the spinal cord relay information to the ventral posterior nucleus within the Thalamus from which there it travels to the somatosensory cortex which responds to painful stimuli and memories of pain (Albanese et al., 2007). Similarly The same area that supports the sensory components of physical pain (secondary somatosensory cortex, dorsal posterior insula) become active. The subcortical circuit that controls defensive response involves processing of stimuli that underlie emotional states associated with persistent pain (Lumley et al., 2009). When the a dysfunctional subcortical defensive circuit interacts with the cerebral cortex it brings forth the conscious experience of fear and anxiety as well as evaluation of the consequences of pain or injury (Johnson, Nolen-Hoeksema, Mitchell, & Levin, 2009).
Central sensitization
[edit | edit source]Central sensitization is characterized by three characteristics: Enhanced pain responses to normally painful stimuli (hyperalgesia), a decrease in pain threshold to normally non-painful stimuli (allydonia), and an increase in spontaneous activity (spontaneous pain) (Lumley et al., 2011.) Persistent pain is mediated by neural plasticity or sensitization within the medial pain system. The medial thalamus relays nociceptive inputs to the anterior cingulate cortex, and persistently stimulates this pathway through pain in the peripheral tissues changing neruons in the cingulate cortex (Shyu & Vogt, 2009)
Pain Relief
[edit | edit source]Pain as said early is an important part of experiencing the dangers in the world. Thus Insensitivity to pain can be dangerous. Individuals with a gene that inactivates pain axons can suffer consequences of repeated injuries and do not learn associative learning of avoiding danger (Johnson et al., 2009). The human mind has been designed to have response dulling terminals to handle pain.
Opioids, Endorphins, and Cannabinoids
[edit | edit source]Once a siginal of pain has been received, continuous pain messages are unnecessary. In response to pain, the brain then stopps prolonged pain through the activation of the opioid receptors. Which functions as system that responds to opiate drugs such as opium (Scherrer et al., 2009). Opiates have been thoroughly studies to bond to these receptors to reduce pain. Endorphins also can help reduce varied types of pain, such as a cut or a burn (Scherrer et al., 2009). Cannabinoids also have a role in pain reduction, as the chemicals related to marijuana, also block certains types of pain. However comparatively to opiates, cannabinoids react mainly in the periphery of the body rather than the central nervous system thus although they do not stop all pain, they at least slow the perception of pain (Scherrer et al., 2009)
Cognition, Emotions, and Pain
[edit | edit source]Pain has been regarded as a catalyst for negative emotional states, pain can cause a disruption in an individuals life that can cause negatively affects to develop (Tan, Jensen, Thornby, & Sloan, 2008). Senses of hopelessness and helplessness can also lead to isolation, sleep disturbances and frustration. These responses increase the likihood of experiencing symptoms similar to depression anxiety and anger. Similar loss of functionality can cause depression as there is a high prevalence of depression among the disability community (Tan et al., 2008). Emotonal states can be represented by many mood disorders such as bipolar, anxiety and depression. Nesse and Ellaworth (2009) have suggested emotional affect works as a functional or evolutionary model which views emotions as potentially facilitating awareness that also guides adaptive behaviors.
Fear-Anxiety-Stress
[edit | edit source]Pain-related anxiety encompasses fearful thoughts about pain, cognitive anxiety symptoms, somatic anxiety symptoms, and escape/avoidance from pain. Research indicates that individuals with elevated pain-related anxiety and fear avoid activities that may be important to recover from acute pain (Lumley et al., 2011). Anxiety and fear as outlined by Rhudy & Meagher (2000)formulate the anticipation of a threat which is characterized by hyper vigilance and passive defensive responses. Fear is elicited by present or imminent threats which motivate defensive responses such as fight or flight. Rhudy & Meagher (2000) research on the use of pain suppressants showed that fear of an external stimulus can inhibit pain in both humans and animals through the activation of endogenous opioids, whereas anxiety increased pain. it was also found that repeated experiences of fear could also elicit anticipatory anxiety, and contribute to persistent pain. As liiterature toward stress and pain increases, psychological distress and trauma have been accepted to be association with persistent pain. Research conducted on childhood and adulthood adversities such as divorce, sexual abuse and physical abuse, indicate a chance of elevating in individuals with various pain conditions such as migraine headaches (Sumanen, Rantala, Sillanmaki, & Mattila, 2007).
Emotional Expression
[edit | edit source]Inidivudals have a varying degree to which they verbally and non-verbally suppress or inhibit their emotions. One major form of process that shows the ambivalence of emotional expression is anger (Lumley et al., 2011). literature has indicated that anger suppression suggest a stronger failure to adaptively express anger which exacerbates pain. A study by Porter, Keefe, Lipkus, and Hurwitz (2005) identified that patients with gastrointestinal cancer who have a heightened ambivalence have a greater associated with greater pain and maladjustment. These individuals reported higher pain behavior and poorer quality of life to those compared with patients with low ambivalence. Further studies have also shown that greater ambivalence of emotional expression relate to higher evaluative and affective pain in patients with low pack pain (Lumley et a;., 2011). This was particularly true as anger inhibition predicted higher pain ratings, where as anger expression predicted lower pain raitings among women with fibromyalgia. (Lumley et al., 2011).
Emotional Experiencing
[edit | edit source]Voluntary access to emotional experiences by using one's emotions to promote better health and functioning have also implication for interventions(Lumley et al., 2011). Techniques utiliting mindfulness and acceptance therapy teaches individuals to be non-judgmental aware of their thoughts, emotions, and sensations they feel(Lumley et al., 2011). Mindfulness techniques are derived from traditional Buddhist meditation which promote love and transform anger into compassion (Lumley et al., 2011). Research within this field of intervention has rapidly increased and appears to have positive correlation for pain reduction (Lumley et al., 2011) A study conducted by Kingston, Chadwick, Meron, & Skinner (2007) found mindfulness training has clinically shown a greater tolerance of experimental pain than techniques like learning guided imagery. Clinically the use of mindfulness-based stress reduction (MBSR) is utlitsed for chronic pain problems. Among the adult population low back pain has shown benefits.
Emotional Modulation
[edit | edit source]Emotional valence refers to the positive-negative quality of an emotion. Arousal describes the intensity or activation of the emotion. in the past it has been commonly thought that negative emotions generally exasibate pain, where as positive emotions inhibnit pain. However laboratory research has identified that emotion's valence interacts with arousal levels to convey it's pain effect. Research has suggested that only high arousal levels will increase pain or conversely a pleasant emotion to inhibit pain. Low arousal regardless of affect of emotion, do not influence pain sensitivity (Rhudy, Barley, & Williams, 2010).
Empathy and Pain
[edit | edit source]empathy is an important role in society as it is necessary for bonding within a relationship. Green, Tripp, Sullivan, and Davidson (2009) found that observers with higher self-reported empathy found that individuals administered experimental pain showed much higher levels of pain. Research conversely also found that high-empathy condition applied to themselves are more intense and unpleasant than people who experience low empathy.Interestinly another study found that observers experiencing empathic distress for a person under going a procedure. Facial expression only manifested when they were instructed to imagine themselves experiencing the procedure, but not when imagining a patients feeling (Lamm, Porges, Cacioppo,, & Decety, 2008).Further research on animals has also produce empathic experience of pain, as rodents both recognize and have emotional reactions to the pain of another rodent (Callahan, Gil, Levesque, & Mogil, 2008).
Integrated models of pain
[edit | edit source]An Integrated pain models identifies pain as both psychosocial and biological process that are tightly interweaved (Lumley et al., 2011). Pain is real regardless of whether peripheral or central abnormalities occur Lumley et al., 2011. The Brain it's self is an organ where pain is experienced and modulated. Comparatively to THE original mind-body dualism THEORY, there has been a shift away from viewing the cause of pain as a singular biological factor or psychological factor (Lumley et al., 2011).
Pain-memory-emotion hypothesis
[edit | edit source]The triangular theory of pain memory emotion, suggests there is an overlap between neural network for pain (Prakash & Colwala, 2011). These networks reside predominatly in the dominant left side of the brain.Patients with chronic pain have shown an increased prevalence of emotional and psychiatric abnormalities in previous research with the leading prevalence in patients with Chronic Daily Headache (CDH) than patients with less frequent headaches (Lumley et al., 2011). There appears to be a reciprocal relation between stress and headaches which indirectly shows excitation of the limbic system stimulates the pain network and also the reverse. Emotional tied memories also have a strong relationship for encoding and being stored. Painful memories may serve as basis for how pain and emotions are fueled by each other with each of the three interacting in a cyclical way (Lumley et al., 2011).
Conclusion
[edit | edit source]Pain is a form of associative learning which teaches individuals to avoid danger. It can occur as acute or chronic pain. Similarly pain has a strong association with emotional affect, as it activates similar centers within the brain including the aCC. Pain also can occur to affect phantom limbs as well as affected limbs. Research has also suggested that mindful techniques have clinical validity in reducing pain. Pain however is a subjective experience of the individual and much can be learnt about the two through a biopsychosocial view.
See Also
[edit | edit source]Chronic Pain and Negative Affect.
References
[edit | edit source]Callahan, B.L., Gil, A.S.C., Levesque, A., & Mogil, J.S.(2008). Modulation of mechanical and thermal nociceptive sensitivity in the laboratory mouse by behavioral state. The Journal of Pain, 9, 174–184.
Cao, Y.Q., Mantyh, P.W., Carlson, E.J., Gillespie, A.M., Epstein, C.J., & Basbaum, A.I. (1998). Primary afferent tachykinins are required to experience moderate to intense pain. Nature, 392,390-394.
DeFelipe, C., Herrero, J.F., O’Brien, J.A., Doyle, C.A., Smith, A.J.H. (1998). Altered nociception, analgesia and aggression in mice lacking the receptor for substance P. Nature, 392, 394-397.
Green, A., Tripp, D., Sullivan, M., & Davidson, M. (2009). Relationship between empathy and estimates of observed pain. Pain Medicine,10, 381–392.
Hadjistavropoulos, T., & Craig, K.D. (2002). A theoretical framework for understanding self-report and observational measures of pain: A communications model. Behaviour Research & Therapy, 40, 551–570.
Kingston, J., Chadwick, P., Meron, D., & Skinner, T.C.(2007). A pilot randomized control trial investigating the effect of mindfulness practice on pain tolerance, psychological well-being, and physiological activity. Journal of Psychosomatic Research, 62, 297–300.
Kross, E., Berman, M.G., Mischef, W., Smith, E.E., & Wagerm T.D. (2011). Social rejection shares somatosensory representations with physical pain. National Academy of Science, 108(15), 6270-6275.
Lackner, J.M., Coad, M.L., Mertz, H.R., Wack, D.S., Katz, L.A., Firth, R., & Lockwood, A.H. (2006). Cognitive therapy for irritable bowel syndrome is associated with reduced limbic activity, GI symptoms, and anxiety. Behaviour Research and Therapy,44, 621–638.
Lamm, C., Porges, E.C., Cacioppo, J.T., & Decety, J. (2008). Perspective taking is associated with specific facial responses during empathy for pain. Brain Research, 1227, 153–61.
Lumley, M.A., Cohen, J.L., Borszcz, G.S., Cano, A., Radcliffe, A.M., Porter,L.S.,Schubiner, H., & Keefe, F.J. (2011). Pain and emotion: A biopsychosocial review of recent research. National Institute of Health, 67(9), 942-968.
Nesse, R.M., & Ellsworth, P.C. (2009). Evolution, emotions, and emotional disorders. American Psychologist, 64, 129–139.
Neugebauer, V., Galhardo, V., Maione, S., & Mackey, S.C. (2009). Forebrain pain mechanisms. Brain Research Review, 60,226–242.
Ploner, M., Gross, J., Timmerman, L., & Schnitzler, A. (2006). Pain processing is faster than tactile processing in the human brain. Journal of Neuroscience, 26, 10879-10882.
Porter, L.S., Keefe, F.J., Lipkus, I.,& Hurwitz, H. (2005). Ambivalence over emotional expression in patients with gastrointestinal cancer and their caregivers: Associations with patient pain and quality of life. Pain 117,340–348.
Prakash, S., & Golwala, P. (2011). Phantom headache: Pain=memory-emotion hypothesis for chronic daily headache? Journal of Headache and Pain, 12, 281-286.
Rhudy, J.L., & Meagher, M.W.(2000). Fear and anxiety: Divergent effects on human pain thresholds. Pain, 84, 65–75.
Rhudy, J.L., Bartley, E.J., & Williams, A.E.(2010). Habituation, sensitization, and emotional valence modulation of pain responses. Pain, 148, 320–327.
Ringel, Y., Drossman, D.A., Leserman, J.L., Suyenobu, B.Y., Wilber, K., Lin, W., & Mayer, E.A. (2008). Effect of abuse history on pain reports and brain responses to aversive visceral stimulation: An FMRI study. Gastroenterology, 134, 396–404.
Scherrer, G., Imamachi, N., Cao, Y.Q., Contet, C., Mennicken, F., O’Donnell, D., et al. (2009). Dissociation of the opioid receptor mechanisms that control mechanical and hear pain. Cell, 137, 1148-1159.
Shyu, B.C.,& Vogt, B.A.(2009). Short-term synaptic plasticity in the nociceptive thalamic-anterior cingulate pathway. Molecular Pain,.5,51.
Singer, T., Seymour, B., O’Doherty, J., Kaube, H., Dolan, R.J., & Frith, C.D. (2004). Empathy for pain involves the affective but not sensory components of pain, Science, 303,1157-1162.
Sumanen, M., Rantala, A., Sillanmäki, L.H., & Mattila, K.J.(2007). Childhood adversities experienced by working-age migraine patients. Journal of Psychosomatic Research. 62, 139–143.
Tan, G., Jensen, M.P., Thornby, J., & Sloan, P.A. (2008). Negative emotions, pain, and functioning. Psychological Services, 5(1), 26-35.
Vogt, B.A. (2005). Pain and emotion interactions in subregions of the cingulate gyrus. Nature Reviews. Neuroscience, 6(7) 533-544.
