Emergency medical responder (EMR)

Introduction
[edit | edit source]Please note that the EMR module is incomplete. Currently no units are completed.
Emergency medical responders can range from bystanders with Cardiopulmonary Resuscitation (CPR) certification to trained professional rescuers such as First Responders, EMT-Basics/Intermediates, Paramedics, Nurses, or Doctors. Usually the most important tool used by these people is their brain. In Alberta, Canada, an EMR is a trained EMS professional, as per the National Occupational Competency Profile (NOCP), equivalent to the EMT-B in the U.S.A. This is also true in British Columbia, Canada. The hierarchy of paramedics in the BC Ambulance Service is highest at the Critical Care Paramedic (CCP), followed by Advanced Life Support (ALS), the Infant Transport Team (ITT), Primary Care Paramedic (PCP), and finally Emergency Medical Responder (EMR).
Preface
[edit | edit source]In general, Emergency Medical Responders are people such as police officer, firefighter or EMT that are trained to provide immediate pre hospital medical treatment to either a medical or trauma victim of accidents or disasters. EMR are not supposed to replace an EMT or Paramedic, EMR’s are only to provide enough care until the ambulance arrives. However, inn Canada, as per the NOCP of the Paramedic Association of Canada, an Emergency Medical Responder (EMR) is the first of four levels of paramedic training. The four levels are Emergency Medical Responder, Primary Care Paramedic, Advanced Care Paramedic, and Critical Care Paramedic (lowest level of training to highest level of training).
Scope of care
[edit | edit source]This is the Scope of Practice for Alberta Canada only. Please look for your specific location to find your scope. EMR Scope of Practice An Emergency Medical Responder may, under medical control and with an ongoing medical audit, provide the following health services: (a) conduct primary and secondary surveys, including scene assessments (b) use basic methods of managing medical, traumatic and obstetrical emergencies (c) use airway management techniques, including oropharyngeal airways, oral suction devices and oxygen-supplemented mask devices to assist ventilation (d) administer oxygen using basic delivery devices including masks and nasal canula (e) basic bandaging (f) cardiopulmonary resuscitation (g) patient extrication (h) use basic splinting techniques, including spinal immobilization with long spine boards and cervical collars (i) automated and semi-automated defibrillation ( taken from Section 9 of the Health Disciplines Act of Alberta Canada.)
Skills practiced
[edit | edit source]
- Primary and Secondary surveys
- Basic airway management
- Oxygen therapy
- Ventilation support
- Circulation support
- Automated defibrillation
- Cardiopulmonary resuscitation
- Spinal immobilization
- Vital sign evaluation
- Respirations
- Pulse
- Blood pressure
- Skin condition
- Pupils
- Blood glucose
- Pulse oximetry
- Splinting
- Bandaging
- Stretcher Operation
- IV Maintenance (starting an IV is a PCP/ACP/CCP skill)
- Patient extrication and transport
Tools used
[edit | edit source]The typical tools used by an EMR include but are not limited to the following:

- Airway management tools:
- Oropharyngeal airways (all sizes).
- Nasopharyngeal airways (all sizes).
- Electric suction, or, V-Vac.
- Yankeur suction tubing.
- Bulb suction.

- Oxygen therapy tools:
- Easyseal mask.
- Simple face mask.
- Non-rebreathing mask (NRB).
- Nasal cannulae.
- Oxygen tubing.
- Compressed, medical grade, oxygen with regulator.

- Ventilation support tools:
- Bag valve mask (BVM).
- Pocket mask.
- Circulation support tools:
- Automated external defibrillator (AED).

- Spinal immobilization tools:
- Long Back board.
- Short Spine board.
- KED.
- C-collar.
- Head roll.
- Scoop stretcher.

- Vital sign evaluation tools:
- Stethoscope.
- Sphygmomanometre.
- Pediatric BP cuff.
- Adult BP cuff.
- Large BP cuff.
- Penlight.
- Pulse Oximetre.
- Blood glucose metre.

- Other tools:
- Traction splint.
- Assorted splints.
- Assorted bandages.
- Stretcher.
Body of knowledge
[edit | edit source]- Human anatomy
- See main unit Human anatomy
- Pharmacology
- See main unit Pharmacology
Standard protocols
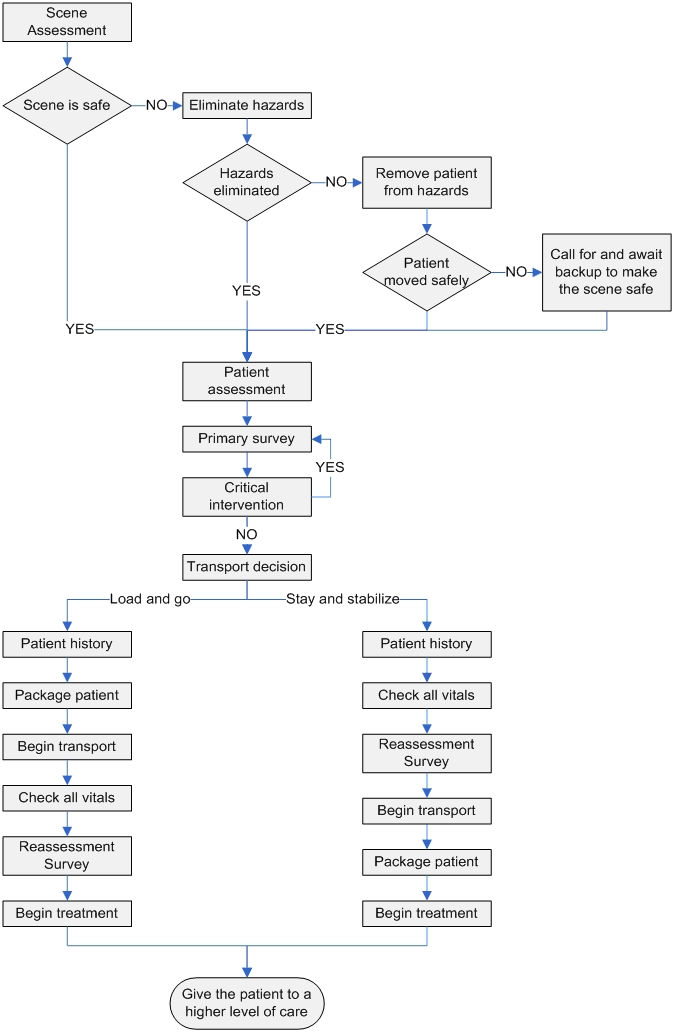
[edit | edit source]The most important thing for any EMR is the systemic approach. For every scene and every patient one must follow the same protocol. This protocol is designed to ensure that all life threatening injuries and illnesses are stabilized with a priority sequence and that none are missed. Failure to follow this protocol could result in the loss of a patient and the revocation of an EMR licence and potentially litigation/prosecution should injury/death result (failure to meet the standard of care). Protocols are part of offline medical control. In certain (rare) circumstances, online medical control (direct call to a medical physician, typically a trauma surgeon or the medical director of the relevant entity) can grant an EMR special permissions.
Scene Survey
[edit | edit source]Upon arriving on scene at any call, an EMR will be required to take certain measures prior to approaching the patient(s) to ensure Responder safety Remember the first priority of every Rescuer/EMR is safety of self and team.
Study the Scene/patient assessment module.
Primary survey
[edit | edit source]
The primary survey is a systemic approach to analyzing the patient in order to rapidly find any life threatening injury or illness. The sequence to be followed is reviewed in the EMR primary survey module and should not be interrupted with the exception of to perform a critical intervention.
Level of Consciousness (LOC)-->Delicate spine/Suspected delicate spine
Airway-->Breathing-->Circulation-->Deadly Bleeding-->External Defib (if necessary)
Rapid Body Survey (RBS)=Head-->neck-->torso/back-->pelvis-->legs-->arms
Study and master the Primary survey module before moving on.
Skin Oxygen(remember to get a baseline SPO2 before throwing O2 on) Airway(as in OPA or NPA) Position of patient

Critical interventions
[edit | edit source]During the primary survey an EMR may find an immediate life threatening emergency. In these cases the EMR will interrupt the primary survey to perform a critical intervention.
Learn what is and is not classified as a critical intervention and how to carry out a critical intervention in the Critical interventions module
Transport decision
[edit | edit source]After the primary survey, an EMR must decide whether it is essential to load and go (load the patient into the ambulance immediately and begin transport), or if the EMR can stay on the scene to stabilize the patient (A.K.A. stay and play).
Study the protocol for the transport decision in the Transport decision module.
Secondary Survey
[edit | edit source]Patient history
[edit | edit source]An EMR must retrieve the same medical history for the patient regardless of the suspected mechanism of injury or illness (MOI).
Study the Patient history module.
Vitals
[edit | edit source]A full set of vitals should include: LOC, RRM(rate/rhythm/quality) of respirations and pulse, skin colour condition and temperature, blood pressure, pulse oximetry, pupils, and blood glucose.
Head-to-Toe
[edit | edit source]A more detailed version of the RBS. Visually assess for any deformities, contusions, abrasions, penetrations, burns, tenderness, lacerations, swelling. Also feel for any tenderness, instability or crepitus. The head2toe should be completed in the following order: Head-->Neck-->Chest-->Abdomen-->Pelvis-->Lower Extremities-->Upper Extremities-->Back
This is the above mentioned mnemonic used for assessing 'head-to-toe'. It is done as it sounds. For whatever trauma pt, it will be DCAP-BTLS. For unconscious, ask any bystanders if they know what happened, how, if others were involved, etc. If they possibly know the pt's medical history or any allergies or conditions. So for unconscious or conscious, this will be used:
D- Deformities
C- Contusions
A- Abrasions
P- Perforations, punctures, penetrations
B- Burns
T- Tenderness
L- Lacerations
S- Swelling
One for the Medical patient will be done by (if awake and conscious), SAMPLE history and if in pain, OPQRST:
S- Signs and Symptoms ("what does your pain feel like?")
A- Allergies ("Do you have any allergies?")
M- Medications ("Are you on any meds? What ones?")
P- Past of medical history ("Have you had this happen before? Do you have any other medical problems?")
L- Last Oral Intake ("What did you last eat?")
E- Events prior and causing EMS to come ("What happened to make you need to call?")
and
O- Onset ("What happened to make you feel this way?")
P- Provocation ("Does anything help it feel better or get worse?")
Q- Quality ("What does your pain feel like?")
R- Region(s)/ Radiating ("Does the pain spread anywhere else? Where exactly does it hurt?")
S- Severity
T- Time and History
Process flow
[edit | edit source]Spinal immobilization
[edit | edit source]Measuring vitals
[edit | edit source]Respirations
[edit | edit source]The respiratory rate (number of respirations the patient makes in one minute) should be measured. Place one hand on the patient’s solar plexus and if the patient is unconscious, hover an ear a few inches above the patient’s mouth. Watch the chest rise and fall while listening to the quality of the breaths. Count the number of breaths taken over one (1) minute, if expedience is necessary, count the breaths over fifteen (15) seconds and multiply the number by four (4).
The number of breaths per minute should be as follows:
- For an adult;
- 12 to 20 breaths per minute.
- If the patients breaths per minute exceed 30 or are below 10 a critical intervention is required.
- 12 to 20 breaths per minute.
- For an adolescent aged 11 to 14;
- 12 to 20 breaths per minute.
- For a child aged 6 months to 10 years;
- 15 to 30 breaths per minute.
- For an infant;
- 25 to 50 breaths per minute.
Sounds to listen for in a patients breathing are.
- Snoring: Indicates a partial blockage of the airway.
- Wheezing: Indicates inflammation in the patient’s airway.
- Gurgling: Indicates fluids in the airway.
- Stridor: Indicates the Larynx is swollen and blocking the upper airway
Breath quality may be observed by looking for the following
- Normal: a normal rise and fall of the chest without accessory muscle use.
- Shallow: a very slight rise and fall of the chest.
- Labored: use of accessory muscles while breathing. In a conscious patient this can be identified by a complaint of “having trouble breathing”.
Pulse
[edit | edit source]The pulse should be measured from the carotid artery in an adult or child, and from the brachial artery in an infant. Place the index and middle figure on the artery to feel the pulse. Count the number of beats per minute, just as the breaths are counted.
A normal pulse rate should be as follows:
- For an adult or adolescent older than 11;
- 60 to 105 beats per minute.
- For a child aged 3 to 10;
- 70 to 130 beats per minute.
- For a small child aged 6 months to 3 years;
- 80 to 140 beats per minute.
- For an infant aged 6 months or less;
- 90 to 140 beats per minute.
- For a newborn;
- 120 to 160 beats per minute.
Blood pressure
[edit | edit source]BP testing is done as part of Vitals in the Secondary Survey. To administer Nitroglycerin (almost exclusively to patients of Angina), the patient MUST have a systolic BP of >100. See Pharmacology.
As of 2016, the systolic BP requirements for NTG administration is now >/= 90 mmhg (Greater than or equal to 90 mmhg) as part of their Chest Pain management protocol in some provinces in Canada, particularly in BC.
Skin condition Pink Warm Dry
[edit | edit source]Pupils PEARL
[edit | edit source]Pupils Equal And Responsive to Light
You can determine this with the medical pen light. (Depends upon the EMS company, sometimes they will provide you one for free or at low cost, or you're going to have to get one yourself.)
Blood glucose 80-120 (Or 3.8mmol/l - 8.0mmol/l)
[edit | edit source]Just remember, four to eight is great!!
Pulse oximetry 90-100%
[edit | edit source]Pulse oximetry uses a light emitter with red and infrared LEDs that shines through a reasonably translucent site with good blood flow. On adults you should place the pulse oximeter on the finger tip(one without finger nail polish if possible). This device measures oxygen saturation in the blood(SpO2). The reading should be in the range of 90-100% for healthy persons. 95% or higher is an ideal SpO2 reading. Anything <80% is basically incompatible with life. This device can tell you whether or not oxygenated blood is being circulated through the body.
Level of Consciousness
[edit | edit source]AVPU [A-Alert] [V-Alert to verbal stimuli] [P-Alert to pain (sternal rub, pinch)]* [U=Unresponsive]
- In British Columbia, Canada, the sternal rub is considered an old standard and no longer Best Practice.
Glascow Coma Scale (GCS)
[Eyes] 4-Spontaneous 3-Responsive to verbal stimuli 2-Responsive to pain stimuli 1-None
[Verbal] 5-Oriented 4-Confused 3-Inappropriate words 2-Incomprehensible sounds 1-None
[Movement] 6-Obeys verbal commands 5-Localizes 4-Withdraws 3-Flexion 2-Extension 1-None
In the Province of British Columbia, Canada, a patient with GCS of 13 or less is RTC (rapid transport category).
Temperature (Tympanic Thermometer)
[edit | edit source]Moving the patient
[edit | edit source]Maintaining spinal immobilization
[edit | edit source]Helmet Removal
[edit | edit source]Though not required if it doesn't impede other protocols, helmets are typically removed by paramedics. This is because hospital staff are typically not trained to properly remove helmets while maintaining spinal stabilization, nor are firefighters and other first responders.
Cervical Collar
[edit | edit source]Patients with a delicate spine are first returned to an anatomical position, including realignment of the head&neck via a 2-axis movement. Thereafter, a hard cervical collar is applied. Note: the cervical collar is not, by itself, considered adequate spinal stabilization.
Spineboard
[edit | edit source]Kendrick Extrication Device (the K.E.D.)
[edit | edit source]Commonly used in auto-vehicle collisions.
Scoop Stretcher
[edit | edit source]In Canada, with the exception of the British Columbia Ambulance Service, the scoop stretcher is (in general) no longer used for spinal stabilization. It is also difficult to use in non-flat&hard surfaces (e.g., snow, dirt, sand...etc.).
You DO NOT remove anything additional (helmet, impaled bar, knife, etc.) unless it interferes with CPR/ airway.
Body mechanics
[edit | edit source]When to move a patient
[edit | edit source]Lifts and carries
[edit | edit source]Stretchers
[edit | edit source]Ambulance stretcher
[edit | edit source]Chair stretcher
[edit | edit source]Identifying and treating illness and injury
[edit | edit source]Medical
[edit | edit source]Respiratory emergencies
[edit | edit source]Cardiovascular emergencies
[edit | edit source]Abdominal emergencies
[edit | edit source]Diabetic emergencies
[edit | edit source]Anaphylactic emergencies
[edit | edit source]Drug and poison emergencies
[edit | edit source]Child Birth
[edit | edit source]Special Populations
[edit | edit source]===Heat related emergencies=== (96.53.108.182 19:07, 13 September 2012 (UTC)Myles Walters96.53.108.182 19:07, 13 September 2012 (UTC)) Three stages, listed from least fatal, to most. 1-heat cramps S/S (signs and symptoms)
-Faintness, dizziness, exhaustion
-rapid pulse
-nausea, possible vomiting
-hot sweaty skin
-sever muscular cramps and pain
2-heat exhaustion S/S
-Pale skin
-Sweaty
-nausea
-shaking
3-heat stroke- disturbance of heat regulating system and lack of sweating. Temperature over normal range. 40*C will develop into cardiogenic shock if untreated. (most people who think they have heat stroke usually have heat exhaustion)
S/S
-temperature rising to 40*C+
-rapid full pulse
-hot dry skin (absence of sweating)
-noisy breathing
-restlessness, convulsions, unconsciousness
Cold related emergencies
[edit | edit source]Cold related emergencies are no where near as dangerous as heat related emergencies. But these emergencies usaully occur in a backcountry or wilderness settings rather than an urban setting. Cold related emergencies can range anywhere from moderate (1st degree) frostbite to Severe (3rd degree) frostibite and to Hypothermia.
Prevention
[edit | edit source]Diagnosis
[edit | edit source]Diagnosis is the single biggest thing an EMR can do. In the case of severly hypothermic patients a pulse may be present but not felt by the EMR. Leading them to believe this person has had a Myocardial Infarcation. If a good history is available it will show that this person has not had heart failure but rather is severely hypothermic. All patients who appear not to have a pulse after checking for 10 seconds or less, MUST receive CPR/Chest Compressions. PUSH HARD, PUSH FAST and ensure a higher level of care is on it's way, usually by calling 911. Any rough handling such as CPR can cause the heart to go into a cardiac arrhythmia such as Ventricular Fibrillation(V-Fib).
Treatment
[edit | edit source]Treatment for the cold injured is dependent upon the condition (frostbite or hypothermia) and severity of the condition. Generally the EMR is not going to treat severe cases of cold injury. The most likely course of action is to bring the patient in to a hospital.
Trauma
[edit | edit source]Shock
[edit | edit source]3 Stages of Shock
Compensated Pale Skin Slightly rapid heart rate Normal blood pressure Anxiety Delayed capillary refill in the infant or child
Decompensated Thirst Rapid heart rate Decreased blood pressure Cool and moist skin that is pale, grey, or bluish and mottled. Major changes in the patient's mental status.
Irreversible Cells start to die. Very low blood pressure Extremley rapid pulse. Death is imminent at this point or stage of shock.
TYPES OF SHOCK: 1.Hypovolaemic shock- Patient has lost enough blood to send them into shock. If not treated immediately, it is fatal. Treat the sourceof the bleeding and transport them to ER. Blood volumizers can be administered through IV(large bore if possible). Hextend or hetastarch can buy time until transfusions and surgical care can be arranged.
2.Cardiogenic shock- This is cardiac pump failure. The heart has been damaged by an acute myocardial infarction, and isn't healthy enough to perfuse the organs of the body. This could lead to cardiac arrest and other organ failure. Patient should be taken to cardiac surgery hospital.
3.Anaphylactic shock- This occurs when a patient comes into contact with something that he/she is severely allergic to. Patient will appear swollen, red and splotchy skin legions, contact dermatitis. The problem is that when this occurs, the patients airway can close up. If the patient can't breathe, they will be dead within minutes. Responder should administer epinephrine immediately, and contact EMS or transport to nearest emergency center. Epi pins or so they are called are emergency auto injectors that people carry, especially if they know they are allergic to certain insect bites. Look for a medical allergy tag. This also tells of medications that the patient is allergic to. If Patient's airwary is closed, EMT must intubate the patient. The Combitube may be a good choice, because it is a blind insertion. Even if you miss the trachea, you can inflate a balloon fixed to the device and your bag valve mask will force O2 down the bronchial main tubes, and into the lungs.(always check for bi-lateral chest movement, and gastric distention)
4.Septic shock - Severe infection starts to shut down the body's organs. Perfusion is decreased to all parts of the body, and if not treated patient will die. Doctors must treat patient with antibiotics and anti-viral medications to save the patients life. However, once a patient has entered septic shock, they are in serious medical trouble.
5.Psychogenic shock - The body loses control over its ability to contract and dilate blood vessels. This could cause a patient to faint, because inadequate levels of blood and oxygen are reaching the brain. This can be cause by shocking news or other traumatic event. The first thing you can do is prevent the patient from injuring themselves when they fall. The skin may appear pale, and the patient may feel lightheaded and confused. Try to reassure them, and transport to hospital if needed.
6.Insulin shock - The patient has become hypoglycemic (low blood sugar) due to excessively high levels of insulin in the blood stream. Patient will be confused, light headed, combative(possibly) and have redder than usual skin(if light skinned). The medic should administer oral glucose (sub-lingual). This helps raise the patient's blood sugar level. They may begin to come out of shock, however they may still need to see a physician. Always check blood sugar if you're diabetic.