Evidence-based assessment/Vignettes/Christopher


HGAPS is finding new ways to make psychological science conferences more accessible!
Here are examples from APA 2022 and the JCCAP Future Directions Forum. Coming soon... ABCT!
~ More at HGAPS.org ~
| Subject classification: this is a psychology resource. |
Christopher
[edit | edit source]
Clinical description
[edit | edit source]Christopher is a 14-year-old White male who lives with his mother and older brother. He is in the accelerated track of courses and skipped a grade. He had been outgoing and popular, and frequently hangs out with his older brother’s friends. He started “hooking up” with women who were friends or acquaintances of his brother. Last year his behavior changed in several ways. He started listening to different music, especially heavy metal, and grunge music. He started dressing differently, wearing spiked leather armbands and boots. Mother reports that he started “hooking” up with girls last year, including older girls who are friends with his older brother. Mom has not confronted him directly about this but believes that he has become sexually active. He has started missing school, sometimes for weeks at a time, complaining of feeling tired and ill, but tests have ruled out bacterial infection and been inconclusive about mononucleosis. The school system has threatened to fail him in all classes for the quarter unless the family can provide a medical explanation for his absences or get him to return to school consistently.
Extended content
|
|---|
History of presenting problem[edit | edit source]Conceptualization[edit | edit source]Initial treatment plan[edit | edit source] |
Assessment findings
[edit | edit source]Checklist scores
[edit | edit source]Christopher, his mother, and his social studies teacher all completed the Achenbach System of Empirically Based Assessment (ASEBA) checklists. Here are the results, reported as T scores (M = 50, SD = 10, compared to other males between 11 and 18 years of age).
| Scale | Mom | Christopher | Teacher |
|---|---|---|---|
| Externalizing | 58 | 53 | 42 |
| Internalizing | 54 | 54 | 56 |
| Anxious/Depressed | 60 | 54 | 54 |
| Withdrawn | 50 | 54 | 50 |
| Somatic Complaints | 54 | 55 | 65 |
| Attention Problems | 86 | 73 | 53 |
| Social Problems | 51 | 54 | 55 |
| Thought Problems | 63 | 70 | 57 |
| Delinquent/Rule-Breaking | 57 | 53 | 50 |
| Aggressive Behavior | 58 | 54 | 50 |
Extended content
|
|---|
Select more specialized scales to refine probabilities[edit | edit source]Updating probabilities[edit | edit source]Critical items[edit | edit source] |
Diagnostic interview findings
[edit | edit source]Diagnoses are based on a LEAD (longitudinal expert evaluation of all data) consensus meeting following a Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS) interview, using DSM-IV criteria. The same interviewer met with Christopher and then his mother, then discussed any differences of opinion with them as needed to use clinical judgment. KSADS results were reviewed with a licensed clinical psychologist to arrive at a final decision.
- Bipolar I (85% confidence)
- Specific phobia - animals (90% confidence)
- ADHD combined (70% confidence)
- Rule out chronic tic (45% confidence)
- Rule out Learning Disability not otherwise specified (30% confidence)
Cognitive and achievement testing
[edit | edit source](Not done as part of the evaluation; may be able to match up information later)
Let's see how we would apply the EBA principles to Christopher:
Shortlist of probable hypotheses
[edit | edit source]Based on Christopher's age and the common clinical issues, here are some possible issues:
- A mood disorder definitely is a leading hypothesis. Within the "mood" category, the hypotheses should consider major depression, dysthymia, and bipolar spectrum disorders, as well as other medical issues that could lead to mood symptoms.
- Substance misuse should be another hypothesis, based again on its prevalence in his age group.
- Conduct problems would be a fourth -- they are not immediately suggested by the description of the presenting problem, but they are common in the age group, and they also can be a risk factor for self harm.
- Attention problems are worth evaluating based on prevalence, though his prior academic performance does not suggest any additional reason for concern.
Christopher's age increases the probability of a mood disorder, as well as substance misuse, and could be consistent with an adolescent-onset conduct disorder. His solid academic performance previously suggests potential resilience.
Below is a worksheet with the DLRs left blank to be filled in. Answers are below.
| Christopher | Common Dx Hypotheses (A) | Starting Prob. (B) | Broad Measure (D) | Cross-informant (E) | Confirmation (G) | Treatment Phase (I), (J), (K) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Base Rate from Merikangas et al. (2010) NCS-A[1] | Scale & Score | DLR | Revised Prob. | EAY Check | Next Test score | DLR | Revised Prob. | Next Test score | DLR | Revised Prob. | K-SADS Interview | |||
| Any Anxiety | Specific Phobia | 0.19 | Specific Phobia - animals (90%) | |||||||||||
| PTSD | 0.05 | |||||||||||||
| GAD | 0.02 | CBCL T | 0.47 | 0.01 | 0.01 | Other measures are better than Achenbach | ||||||||
| Panic Disorder | 0.02 | |||||||||||||
| Social Phobia | 0.09 | |||||||||||||
| Separation Anxiety | 0.08 | |||||||||||||
| Any Impulse Control Disorder | ODD | 0.13 | CBCL T
Aggressive 58 |
4.18 | 0.38 | 0.38 | No data about TRF scales for aggressive | |||||||
| CD | 0.07 | CBCL T
Aggressive 58 |
4.18 | 0.24 | 0.24 | |||||||||
| ADHD | 0.09 | CBCL T
Attention 86 |
6.92 | 0.41 | 0.41 | TRF T
Attention 53 |
0.73 | 0.34 | ADHD combined (70%) | |||||
| Any Mood Disorder | MDD | 0.12 | CBCL T
Anx/Dep 60 |
3.78 | 0.34 | 0.34 | Haven't found data about TRF for internalizing | |||||||
| BP | 0.03 | CBCL T | 0.53 | 0.02 | 0.02 | YSR T
Externalizing 53 |
0.52 | 0.01 | TRF T
Externalizing 42 |
0.25 | 0.00 | Bipolar I (85%) | 7 Up 7 Down Inventory (Christopher) | |
| CMRS-10(Parent) | ||||||||||||||
| Dysthymia | Included above | |||||||||||||
| Any Substance Abuse Disorder | 0.11 | CBCL #2 CBCL #99 CBCL #105 | ||||||||||||
| Answers | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mention that these have DLRs. Also unpack the implications of agreement and disagreement for the client (and add a section about treatment implications of disagreement on the Conceptual Model Pages)
Mental status and clinical observations
[edit | edit source](add content)
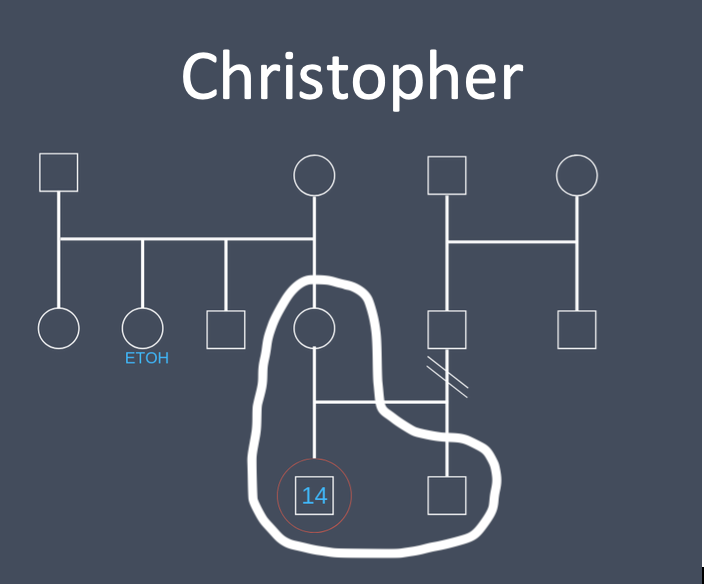
Genogram and family functioning
[edit | edit source]Here is a genogram of Christopher's family:
The diagnostic interview suggests found evidence of a prior manic episode, indicating a diagnosis of bipolar I. This suggests that the periods of low energy and cognitive functioning could be depressive episodes, and interviewing confirmed that they would meet diagnostic criteria for a major depressive episode even though Christopher did not describe himself as "depressed." They clearly were associated with impairment and should be a major focus of treatment.
***
Reliable change index
[edit | edit source]Pick a treatment target and specify what the RCI would be for it. Discuss how you would explain to Christopher.
The treatment target we picked was the self-report of attention problems. For reliable change to be demonstrated with 95% confidence, a decrease of 9 points to 62 would have to be seen.
Nomothetic benchmarks
[edit | edit source]A, B, Cs of Jacobson definitions. General stuff about limitations would go on the main concept page. Here it is focused on the client -- what are the benchmarks they will focus on? How explained to them?
For self report attention problems, to reach the A, B, and C benchmarks, Christopher's scores would have to decrease to:
A- 45
B- 66
C- 58
Interpreting benchmarks
[edit | edit source]Minimum important difference (MID)
[edit | edit source]Note that this section is a dangler -- not originally called out in the 12 steps. Medium d as a rule of thumb from Streiner, Norman, & Cairney (2015). Could work from AUC to d to raw units as a way of estimating, since psychology hasn't done research on this yet. Might be able to back into it with studies that had CSQ and outcome data.
Client goals & tracking
[edit | edit source]These would be personal goals and idiographic measurement -- YTOPS, etc.
This would be traces such as coming to sessions, doing homework assignments. (Not sure of other specifics involved in current IPT protocols?)
YTOPS again and goal setting.
Revisit Jacobson benchmarks. Is there much chance of relapse? What things would the client need to pay attention to if they were going to nip that in the bud?|}
References
[edit | edit source]- ↑ 1.0 1.1 Merikangas, Kathleen Ries; He, Jian-ping; Burstein, Marcy; Swanson, Sonja A.; Avenevoli, Shelli; Cui, Lihong; Benjet, Corina; Georgiades, Katholiki et al.. "Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A)". Journal of the American Academy of Child & Adolescent Psychiatry 49 (10): 980–989. doi:10.1016/j.jaac.2010.05.017. PMID 20855043. PMC PMC2946114. https://dx.doi.org/10.1016/j.jaac.2010.05.017.