Motivation and emotion/Book/2015/Depression in older adults
What are the risk factors for depression in older adults and what can be done about it?
Overview[edit | edit source]
Globally, there is an ageing population. Between 2015 and 2050 there it is estimated that the age of people over 60 years will double. Mental health and well-being are just as important in older adulthood then at any other age (WHO, 2015).
Depression is a major cause of mental illness in older adults as it can have negative effects on daily functioning and cause great suffering to the individuals mental health as well as physical health and also the society as older adults still contribute majorly through family, volunteering and still working in the work force (WHO, 2015). Unipolar depression effects about 7% of the elderly population. Depression in this age group can be both underdiagnosed and undertreated as symptoms are often overlooked because they coincide with other problems associated with older adults. Depression can lead to poorer functioning then those suffering with chronic medical conditions leading to higher utilisation of medical facilities and costs (WHO, 2015). These results show that this is a major issue and further research is needed to combat this issue.
What is Depression?[edit | edit source]
The World Health Organisation’s definition of depression – “a common mental disorder, characterised by sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, feelings of tiredness, and poor concentration” (WHO, 2015).
Depression can be long lasting and impair ability to function at work or in everyday activities (WHO, 2015). It is a condition that impairs an individual’s quality of life and productivity and can in turn lead to further chronic diseases causing economic losses for the individual and also for the community (Onat, Delialioglu, & Ucar, 2014).
Risk Factors[edit | edit source]
In addressing and seeking out some of the causes of depression in older adults, it allows improvements to be made in these areas to prevent these risk factors from causing more harm for the individual and also on society.
Physical Decline[edit | edit source]
In a study by Snowson and Fleming (2008), they found out that the five factors most highly related to depression in people living in nursing homes included sadness over loss of opportunities and ability to participate in valued activities, not being able to help others, and attending but not being able to take part in activities. All of these things relate to physical decline that comes with old age meaning that it is a very major risk factor of depression.
In a study by Wassink-Vossen et al., (2014), it was confirmed that depression in older adults is associated with lower physical activity. Although, this physical inactivity in older adults could be due to functional limitations, being in aged care facilities, and types of medications they are on (wassink-Vossen et al., 2014). To improve physical activity in older adults to improve depression statistics in older adults, specialised exercise programs need to be implemented, targeted to the individuals needs and capabilities.
Living Arrangements[edit | edit source]
Aksullu and Dogan (2004) as cited in Onat, Delialioglu and Ucar (2014) found through their research that there was much higher depression signs seen in those who lived in nursing homes compared to those living in their homes. This could be due to the fact that they have problems settling in as it is such a big change to the life that older adults were previously used to (Snowson & Fleming, 2008).
It has also been reported that depression is underdetected and undertreated in nursing homes (Snowson, & Fleming, 2008). This is a significant problem as many older adults go into nursing homes when they are no longer able to look after themselves. As mentioned above, there are a higher number of older adults with depression in nursing homes. This move in itself could lead to depression as it is a big change in their lives and can also make them feel alienated from family and friends, as well as society in general, leading to depressive symptoms (Winningham, 2007). Also, considering depression isn’t being treated to a sufficient standard, a large number of older adult could be suffering and not getting the support they need.
Loneliness[edit | edit source]

Loneliness is a subjective feeling and can also be experienced in the presence of others (Holvast, Burger, De Waal, Van Marvijk, Comijs, & Verhaak, 2015). In a year, one in ten people will experience loneliness and as people age, the risk of suffering from loneliness increases (BeyondBlue, 2015). This could be due to death of loved ones and also a lack of contact with family and friends who may be busy or a move into an aged care facility can lead to social isolation (Holvast et al., 2015).
Although loneliness can be associated with poorer outcomes for depression, depression can also cause loneliness (Holvast et al., 2015). This is something that people also need to be aware of to prevent the negative impacts of loneliness on the individual and help them overcome depression without any other factors in the way. Chao (2011) reported that having a larger social network and frequently keeping in contact with family and friends can lead to a reduction in depressive symptoms. So maintaining good social connections and having meaningful contact with others can help to prevent loneliness (BeyondBlue, 2015). This will be discussed further under the Prevention and Intervention section of this chapter.
Lifestyle and Behavioural Choices[edit | edit source]
Physical Activity[edit | edit source]
As people age, they often become less physically active due to illness and injury. Physical inactivity has been linked to depression in older adults (Wassink-Vossen et al., 2014). This could be due do many factors. functional capabilities may be affected due to illness or injuries meaning the depressive symptoms could stem from the fact that they are ill or injured (wassink-Vossen et al., 2014). Also if individuals were once extremely active but they are unable to participate in the same activities at their current age it could lead to issues with low self esteem or lack of confidence which are symptoms of depression.
Phillips (2015) reports that when given the option of recreational physical activity programs or walking, patients chose walking. This could be because this is most familiar to them or they feel comfortable with this. It could also mean they are afraid of suffering an injury. Phillips (2015) also states that when older adults move into aged-care facilities they do not appreciate the need for physical activity as the environment they are now in caters for their functional limitations and disabilities. Aged care facilities need to continue to promote physical activity as a tool to limit the risk of older adults suffering from depression.
Drugs and Alcohol[edit | edit source]
Older adults may turn to alcohol or drugs during a difficult time such as a loss of a family member or friend. this could in turn lead to an addiction. Levola, Holopainen and Aalto (2011) found that there is a positive association between depression and heavy drinking. People who drank more heavily had a higher risk of depression. This could be due to the fact that both drugs and alcohol can be addictive, so when the individual with the addiction does not have their drugs or alcohol in their system, they may have feelings of depression. In terms of drugs, it has been revealed that depression is more strongly associated with substance dependence instead of substance abuse (Ferigolo, Stein, Fuchs, & Barros, 2009). When drugs are used in early life, there is a higher chance of developing depression in older adulthood.
Alternatively, it has also been proven that substance abuse and alcoholism develop as a means to cope with depression (Ferigolo et al., 2009). This means that aged care facilitators need to carefully look for signs and symptoms of both depression and/or drug and alcohol abuse in order to prevent the other from occurring.
Diet[edit | edit source]
Evidence suggests that diets rich in fruits, vegetables, wholegrains and fish is associated with a lower risk of depression (Chan, Chan & Woo, 2014). Chan, Chan and Woo (2014) explains that this is due to the antioxidant compounds in fruit and vegetables that can reduce neuronal damage caused by oxidative-stress. Also, long-chain omega 3 polyunsaturated fatty acids found in fish can affect mood by a change of the brain serotonergic function and its immune-neuroendocrine effects. Because many older adults are living in care provided facilities, they cannot choose what they are eating so therefore may not be getting the nutrients that they need as an individual. Also, due to being retired they may have less money to spend on getting all of the needed dietary requirements.
Related Theories and Models[edit | edit source]
Maslow’s hierarchy of needs in relation to depression in older adults[edit | edit source]
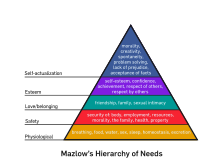
Maslow’s hierarchy of needs theory is about understanding how an individual’s quality of life is related to how well their needs are being met (Timonen & O’Dwyer, 2009). Maslow suggests that needs are hierarchical with physiological needs taking precedence over psychological.
The results from the study by Timonen and O’Dwyer (2009) found that individuals living within a residential care unit were not reaching there physiological needs in terms of lack of sleep, lack of warmth, poor quality of food. Safety needs is also a major concern with patients not feeling like they are receiving enough care in terms of illness or injury, they also don’t feel this new facility feels like a home, suggesting the sense of stability and security is not there (Timonen & O’Dwyer, 2009). Relating to love and belonging needs, the residents often feel lonely and not as connected with family and friends as they were when they were not in the facility. Esteem needs were also not always met as sometimes the staff members speak to the residents in a derogatory way and there is sometimes a lack of respect which can lead to loss of confidence (Timonen & O’Dwyer, 2009).
As maslow explains, to reach the highest stage of self-actualisation, people need to first fullfill all of the lower needs. Considering many older adults – especially those in care facilities have lacked complete fulfilment in the other stages, they will not be able to reach the needs of self-actualisation or some of the other psychological needs if the lower stages have not been met. This in turn could lead to depressive symptoms in this age group.
Another reason for older individuals suffering to meet the psychological needs could be due to physical incapability’s as they are not able to individually satisfy their needs without help. This may cause frustration due to the limited capacity to change their circumstances (Timonen & O’Dwyer, 2009).
Model of Social Support[edit | edit source]
Model of social support
A research study by Chao (2011) looks at social support and depressive symptoms in older adults. They came up with a predictive model of social support which has seven components – social network size, social network composition, frequency of social contact, proximity, types of support, helping others, and satisfaction with support received (Chao, 2011). They used this model in their own study with the results shown in the table below:
Model of the seven components of social support in action
|
Social support component |
Results from Chao’s (2011) study |
|
Social network size |
The bigger ones social network size the less depressive symptoms shown |
|
Social network composition |
Having a diverse social network sees less depressive symptoms |
|
Freq of social contact |
Face to face communication is associated negatively to depression |
|
Proximity |
Living with another relative (or very close to) is associated with lower depression |
|
Types of support |
Received emotional support from loved ones is related to less depressive symptoms |
|
Helping others |
Being able to help others financially is related to lower depression levels |
|
Satisfaction with support |
This is unique to each individual the support each received |
This model can be used in future research studies to extend on the results found in the study by Chao (2011) and it can also be used by people working with older adults to try and assess their levels of depression.
Prevention and Intervention[edit | edit source]
Detection[edit | edit source]
The Cornell Scale for Depression in Dementia (CSDD) and the 15-item Geriatric depression scale (GDS-15) can be implemented into nursing homes to enable carers to identify patients who may be suffering from depression so they are able to come up with a plan to help them, including referring these results onto the patients' general practitioners (Snowson & Fleming, 2008). Training aged-care facilitators to be able to detect symptoms of depression in older adults is an option so they are able to help the individuals suffering to seek help as soon as possible (WHO, 2015).
Physical Activity[edit | edit source]


Physical inactivity has been proven to be a risk factor leading to depression in older adults (Wassink-Vossen et al., 2014). The results in the study by Wassink-Vossen et al (2014) suggest that interventions need to be aimed at increasing this physical activity in older adults by implementing psychotherapeutic interventions to strengthen a sense of mastery and also to overcome function limitations. Programs specialised to the individuals needs and capabilities also need to be implemented to get older adults to do some physical activity that is relevant to their lifestyle (Wassink-Vossen et al (2014). This can therefore lower the risk of suffering from depression.
In their study, Loprinzi (2013) found that even light-intensity physical activity is related to lower depressive symptoms. This means that if older adults are unable to do as much physical activity as they used to due to physical decline in more recent years, even light and lower amounts of physical activity will still have benefits so this needs to be promoted to this age group.
Socialising Activities to use in Aged-Care Facilities[edit | edit source]
As discussed earlier in this chapter, social isolation can occur when older adults move into aged care facilities as they become alienated from friends and family (Winningham, 2007). In their report, Winningham (2007) suggested possible activities to implement into aged care services to facilitate social support networks. Some possible suggestions by Winningham (2007) are listed below:
- Pair residents with similar interests and cognitive functioning allowing them to interact with one another
- Providing name tags and also making a list of everyones names with a picture of themselves for everyone to see to get to know everyone
- Giving residents volunteer or part time jobs within the facility to stay active and interact with others from with the facility as well as visitors.
- Work on puzzles as a group or setting up a book club to build connections with each other as well as improving cognitive functioning
- Day trips to senior centres
- Playing memory games with the residents to reminisce on past memories as well as maintaining good memory functioning
Health Promotion[edit | edit source]
Mental health in older adults can be improved by promoting healthy and active lifestyles (WHO, 2015). Who (2015) recognises that mental health promotion is dependent on strategies to ensure older adults have resources to reach their basic needs. Some options from WHO (2015) are outlined below –
- Providing security and freedom, which also involves having access to housing through a supportive housing policy.
- Social support needs to be available for both individuals and carers
- Community development programs should be implemented
- And health and social programs targeted at those in vulnerable groups or who are in need of mental health support
| RUOK? This little question can make a big difference. R U OK day is an Australia-wide health promotion campaign aimed at providing awareness and helping those in need seek help. |
Future interventions and continuous support[edit | edit source]
WHO (2015) provides some options for interventions and continuous support needed:
- Early diagnosis detection and management of depression
- Increasing and maintaining physical and psychological health and wellbeing
- Provide individuals as well as care givers with long-term support and every individual should have equal access to this support
Treatment[edit | edit source]
There are many different treatments for depression, but the important thing is finding the right one for each individual (BeyondBlue, 2015).
Cognitive Behavioural Therapy[edit | edit source]
A treatment that recognises that a persons way of thinking and behaving affects the way they feel (BeyondBlue, 2015). it is a very effective therapy for depression, especially in older adults.
Antidepressants[edit | edit source]
Antidepressants can be prescribed and it most effective along with psychological therapy (BeyondBlue, 2015). It is very important that each individual goes through the careful process of finding an effective antidepressant that works for them with their GP or psychiatrist. Individuals will need to take into account such things like medical history, age, symptoms and gender (BeyondBlue 2015).
Conclusion[edit | edit source]
Although the risk of major depression in older adults is quite low, the prevelance of depressive symptoms increases with age (Levy-Gigi & Keri, 2015). This could in turn lead to depression if left undetected so it is a very important topic.
There are many risk factors leading to depression in older adults that everyone needs to be aware of such as physical decline, living arrangements, loneliness, and lifestyle and behavioural choices. The preventative strategies such as detection, physical activity, socialising activities and health promotion then need to be put into action in order to improve this issue in the years to come to decrease the number of older adults suffering from depression within this ageing population.
For the future, more extensive research is needed and support services need to be implemented for this age group suffering depression to be able to age happily and healthily.
See Also[edit | edit source]
- Motivation and emotion/Book/2014/Self esteem and depression
- Ageing and intellectual disability
- Motivation and emotion/Book/2013/Dementia and emotion
- Motivation and emotion/Book/2014/Depression and motivation
References[edit | edit source]
Chan, R., Chan, D., & Woo, J. (2014). A prospective cohort study to examine the association between dietary patterns and depressive symptoms in older Chinese people in Hong Kong. Plos ONE, 9(8), 1-11. doi: 10.1371/journal.pone.0105760
Chao, S.F. (2011) Assessing social support and depressive symptoms in older Chinese adults: A longitudinal perspective. Aging & Mental Health, 15(6), 765-774. doi:10.1080/13607863.2011.562182
Connections matter: helping older people stay socially active. (2014). Retrieved from the BeyondBlue Website: http://resources.beyondblue.org.au/prism/file?token=BL/1366
Ferigolo, M., Stein, A. T., Fuchs, F. D., & Barros, H. T. (2009). Influence of depression and early adverse experiences on illicit drug dependence: A case-control study. Revista Brasileira De Psiquiatria, 31(2), 106-113.
Holvast, F., Burger, H., De Waal, M.W., Van Marvijk, H.J., Comijs, H.C., & Verhaak, P.M. (2015). Loneliness is associated with poor prognosis in late-life depression: Longitudinal analysis of the Netherlands study of depression in older persons. Journal of Affective Disorders, 185, 1-7. doi: 10.1016/j.jad.2015.06.036
Levola, J., Holopainen, A., & Aalto, M. (2011). Depression and heavy drinking occasions: A cross-sectional general population study. Addictive Behaviours, 36(4), 375-380. doi: 10.1016/j.addbeh.2010.12.015
Levy-Gigi, E., & Keri, S. (2015). The interactive effect of negative reversal learning and age on depression: Possible cognitive mechanisms underlying the elevated depressive symptoms in older adults. Psychology and Aging, 30(2), 341-347. doi: 10.1037/a0039181
Loprinzi, P. D. (2013). Objectively neasured light and moderate-to-vigorous physical activity is associated with lower depression levels among older US adults. Aging & Mental Health, 17(7), 801-805. doi: 10.1080/13607863.2013.801066
Medical treatments for depression. (2015). Retrieved from BeyondBlue Website: https://www.beyondblue.org.au/the-facts/depression/treatments-for-depression/medical-treatments-for-depression
Mental health in older adults. (2015, September). Retrieved from World Health Organization web site: http://www.who.int/mediacentre/factsheets/fs381/en/
Onat, S.S., Delialioglu, S. U., & Ucar, D. (2014). The risk of depression in elderly individuals, the factors which relation to depression, the effect of depression to quality of life. Turkish Journal of Geriatrics / Türk Geriatri Dergisi, 17(1), 35-43.
Snowson, J., & Fleming, R. (2008). Recognising depression in residential facilities: an Australian challenge. International Journal of Geriatric Psychiatry, 23(3), 295-300. doi: 10.1002/gps.1877
Timonen, V., & O’Dwyer, C. (2009). Living in institutional care: residents’ experiences and coping strategies. Social Work in Health Care, 48(6), 597-613. doi: 10.1080/00981380902791267
Wassink-Vossen, S., Collard, R.M., Voshaar, R.O., Comijs, H.C., De Vocht, H.M., & Naarding, P. (2014). Physical (in)activity and depression in older people. Journal of Affective Disorders, 161, 65-72. doi: 10.1016/j.jad.2014.03.001
Winningham, R.L. (2007). A cognitive intervention to enhance institutionalized older adults’ social support networks and decrease loneliness. Aging & Mental Health, 11(6), 716-721.
External links[edit | edit source]
- Beyond Blue - Life starts at 60
- Beyond Blue - Connections matter
- Here are two clips from a Beyond Blue campaign targeted at older adults to encourage them to seek help when needed and to show them that things can get better *Dale's Story *Brian's Story
- WHO - Mental Health and Older Adults
- Lifeline
- Black Dog Institute